Brachytherapy
Home > Clinical Concepts In Radiation Oncology > Radiation Tissue Tolerance > Treatment Options > Brachytherapy
Can we please get your advice on this one question?
Brachytherapy is a form of radiotherapy where a sealed radiation source is placed inside or next to the tumor.
Brachytherapy is classified according to:
- Location of implants
- Type of loading
- Dose rate
- Duration of treatment
- Type of emission.
Types of brachytherapy according to location of implants
Three common techniques of radioactive implants applied in brachytherapy:
- Molds/ plaques: Molds or plaques are used for superficial lesions whereby the
radioactive source is placed on the skin 1-2 cm from the lesion. It is mostly
used in treating tumors of the eye.
- Interstitial: Interstitial implant involves temporary placement of a radioactive source into the tumor volume example in a breast tissue.

Interstitial Breast Implant
- Intracavitary: In intracavitary implant, sealed radioactive source is placed in the body cavity. Cancer of the cervix, uterus and vagina are often treated by this procedure. A cervical applicator consists of central tube (tandem) and lateral capsules (ovoids).
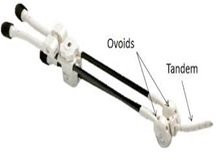 A Cervical Applicator |
 A Vaginal Applicator |

Intracavitary Procedure on Cancer of the Cervix
Types of brachytherapy loading
1. Manual
afterloading: The radiation sources are manually
afterloaded into aplicators or catheters that have been placed within the
target volume. At the end of the treatment the sources are removed gain. The
manual loading and offloading of the radiation source result into high
radiation exposure to the medical staff.
2. Remote afterloading: In remote afterloading, machines or systems automatically administer a radiation source directly to the tumor minimizing radiation exposure to the medical staff and to the surrounding normal tissue.

Remote afterloading technique
Types of brachytherapy emission
Brachytherapy classification with respect to Dose Rate
There are two main types of dose rates:
- Low Dose Rate (LDR) (0.4-2.0 Gy/h): Low Dose Rate is mostly used where radioactive seeds are permanently implanted into the tumor.
- High Dose Rate (HDR) (>12 Gy/h): High Dose Rate is mostly used where radioactive seeds are temporarily implanted into the tumor or placed close to the tumor
Duration of Treatment
- Permanent implant: In a permanent implant, radioactive source remains in the tissue indefinitely. Short half-life isotopes are used, example; I-125, Pd-103, Au-198.
- Temporary implant: In a temporary implant, radioactive source is removed from patient within a short period of time once desired dose has been delivered.
Principles of Brachytherapy:
- Brachytherapy has higher Tumor Control Probability due to higher tumor dose.
- There is lower dose to surrounding normal tissue.
- Morbidity and complications increase when treating large volumes, thus the treatment volume is minimized.
- Total treatment duration is kept minimal because shorter time intervals between treatments reduce repopulation of tumor cells.
Advantages of Brachytherapy
- Sharp dose fall-out outside the target volume because of attenuation by inverse square law hence minimizing dose to the surrounding tissue.
- Short duration of treatment (20-70 Gy in 2-7 days) unlike EBRT which takes 4-7 weeks.
- Improved localized dose delivery to the target.
- Continuous radiation by LDR allows redistribution of cells in cell cycle.
- Better conformal therapy since dose distribution can be manipulated to make irregular shaped tumors.
Disadvantages of Brachytherapy
- It is only suitable for well localized tumors.
- There is no therapeutic dose due to positive surrounding lymph nodes.
- Sharp dose fall-off might not adequately cover tumor volume.
- Great risk of late complications using HDR given with inadequate fractionation.
- Requires special skills and training.
The most commonly used systems in Brachytherapy:
- Quimby (Memorial) System: In this system, the radioactive sources are distributed uniformly over a plane or a volume of tissue. The dose near the center of the implant is much greater than at the edge of the implant. Thus in Quimby system, a uniform distribution of radioactive sources is used to give a non-uniform dose distribution.
- Manchester (Patterson-Parker) System: In
Manchester system, the radioactive sources are distributed non-uniformly over
the area or the volume of the implant to give a uniform dose distribution. The
aim of the system is to deliver a uniform dose of ± 10 % in the implanted area
or volume.
- Paris System: Paris
system was developed for linear sources of iridium wire. It is used for single
or double plane implants. In this system, sources are distributed uniformly for
a planar implant but follow a particular pattern for volume implants.
Internal radiation therapy is a form of treatment where a source of radiation is put inside your body. One form of internal radiation therapy is called brachytherapy. In brachytherapy, the radiation source is a solid in the form of seeds, ribbons, or capsules, which are placed in your body in or near the cancer cells. This allows treatment with a high dose of radiation to a smaller part of your body. Internal radiation can also be in a liquid form. You receive liquid radiation by drinking it, by swallowing a pill, or through an IV. Liquid radiation travels throughout your body, seeking out and killing cancer cells.
Radioactive isotopes used in brachytherapy:
The radioactive isotopes in brachytherapy,
Name Half-life
1. Radium 226 1600 years
2. Iridium 192 73.8 days
3. Cobalt 60 5.26 years
4. Cesium 137 30 years
5. Gold 198 2.7 days
6. Iodine 125 59.4 days
7. Radon 222 3.83 days
Various techniques used in brachytherapy:
Brachytherapy sources are applied in three ways: external applicators or molds, interstitial implantation, and intracavitary therapy (fig a). A choice of one technique or the other is dictated primarily by the size and location of the tumor. For example, surface molds are used to treat small superficial areas, such as the ear or the lip; interstitial therapy is indicated when the tumor is well localized and can be implanted directly according to accepted rules of distribution; intracavitary therapy is used when applicators containing radioactive sources can be introduced into body cavities. In all these cases, owing to the short treatment distance, the geometry of source distribution is critical.
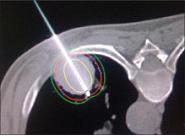

Figure a shows the images various techniques used in brachytherapy
Brachytherapy may be used with people who have cancers of the head, neck, breast, uterus, cervix, prostate, gall bladder, esophagus, eye, and lung. Liquid forms of internal radiation are most often used with people who have thyroid cancer or non-Hodgkin's lymphoma. You may also get internal radiation along with other types of treatment, including external beam radiation, chemotherapy, or surgery.
Questions:
1. Brachytherapy will used for the cancer of
a) Cervix
b) Breast
c) Tongue
d) Oesophagus
e) All
Answers:
1. e) All
References:
1. http://www.thegreenjournal.com
3.http://www.cancerjournal.net/articles/2011/7/2/images/JCanResTher_2011_7_2_174_82914_u2.jpg
4. http://radiographics.rsna.org/content/25/4/1119/F46.medium.gif
5. The Physics of Radiation Therapy by F.M.Khan
Home > Clinical Concepts In Radiation Oncology > Radiation Tissue Tolerance > Treatment Options > Brachytherapy
FREE Infographic What successful people believe. What successful people do
Dictionary of Cancer Terms
Need help understanding a word? Here is an electronic resource that gives meaning to Cancer terms and their usage.
StrengthsFinder 2.0