Medical Emergencies
Home > Patient Care And Education > Medical Emergencies
- Allergic Reactions
- Cardiac or Respiratory Arrest
- Physical Injury or Trauma
- Physical Injury or Trauma
- Other Medical Disorders
Four; 4 questions out of the 30 questions in the Patient Care and Education content area come from the Medical Emergencies sub-topic
Can we please get your advice on this one question?
Allergic ReactionsCardiac or Respiratory Arrest
Physical Injury or Trauma
Other Medical Disorders
- Allergic Reactions
An allergic reaction is a reaction (or immune response)
to a substance that is not usually harmful.
Let’s review some items found in a Radiation Therapy department that have the potential to cause allergic reactions. The reactions may be local as well as minimal in terms of itching, swelling, and /or hives or the allergic reaction may become whole-body as well as severe which is called anaphylaxis. Anaphylaxis is a rapid serious reaction which may cause death from an itchy rash, throat swelling (an inability to breathe), and low blood pressure.Here is a picture of what hives look like:

Here is a picture of what anaphylaxis looks like. (This is a medical emergency; seek immediate assistance with this patient)
Patients have a right to report any adverse reactions to the Food and Drug Administration's (FDA) MedWatch Adverse Event Reporting program by phone at by phone 1-800-332-1088 and online at http://www.fda.gov/Safety/MedWatch
- Latex Gloves
Latex gloves are commonly used in health care environments. Allergic reactions to a protein found in the latex gloves means that these gloves maybe replaced with non-latex gloves. Allergic reactions commonly take the form of localized swelling as well as itching. Before handling patients with latex gloves ask them if they are allergic to latex.
- Tape Adhesive
Tape adhesive is found in band aids as well as silk (medical) tape which is commonly found in health care environments. Allergic reactions commonly take the form of localized swelling as well as itching. Ask patients if they are allergic to adhesive tape before using medical tape on a patient. Paper tape may be used as an alternative.

- Tattoo Ink Marks
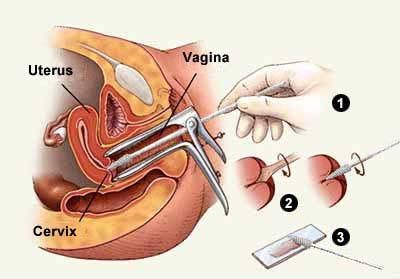
A few pin point tattoo ink marks are normally made during Radiation Therapy simulation to allow Radiation Therapists to setup as well as direct radiation beams. These marking are about a millimeter small approximating a head of a pin in size. Localized swelling reactions may result and should be disclosed in the consent.

- Barium Sulfate
Barium is opaque white, odorless, and of high density making it an ideal radiographic suspension. Barium is commonly used during CT scan simulations to study the gastrointestinal tract. Barium has the consistency of a milk shake and is usually consumed by mouth some 90 minutes to two hours prior to the simulation procedure. Barium may also be given by rectal enema. Barium soaked gauze is also used in Radiation Therapy as a vaginal marker or rectal marker. Reported side effects of barium (some of which may be allergic) include diarrhea, nausea, vomiting, constipation, hives, itching, sweating, confusion, as well as difficulty breathing & swallowing. Notify the supervising clinician if any side effects are observed. http://www.nlm.nih.gov/medlineplus/druginfo/meds/a606010.html
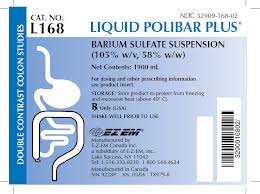
Gastrograffin is an alternate oral / rectal contrast media used for patients who have barium sulfate tolerance issues.http://www.medsafe.govt.nz/profs/datasheet/g/Gastrografinoralrectalsusp.pdf
- Contrast Media Use
A large number of radiographic studies are conducted with contrast media. Have a look at this extensive National Cancer Institute list of Radiographic Examinations Using Contrast Media. http://training.seer.cancer.gov/abstracting/procedures/clinical/radiologic/contrast.html
Cystograms (an x-ray visualization of the urinary bladder using an injection of contrast) are a commonly performed study in the Radiation Therapy department. An ionic contrast media is often used but maybe substituted for non-ionic contrast for patients who are allergic to iodine.
In practice, patients are often asked if they are allergic to shellfish as this was thought to correlate to an iodine allergy. We now know that an allergy to shellfish may not necessarily mean the patient is allergic to iodine contrast.
https://acaai.org/resources/connect/ask-allergist/shellfish-allergy-related-iodine
Oral / rectal as well as intravenous (or IV) contrast may be prescribed for a Cat Scan simulation examinations in the Radiation Therapy department. Oral / rectal contrast as we have discussed allows the visualization of the gastrointestinal systems. IV contrast by comparison has the ability to highlight tissues, organs, as well as blood vessels. Cancer tends to create additional blood vessels (angiogenesis) to fuel its uncontrolled growth (http://www.angioworld.com/cancer.htm) which are better visualized using IV contrast.
Blood studies; namely BUN (Blood Urea Nitrogen), creatinine, and GFR are routinely ordered prior to the administration of intravenous contrast for certain patient populations. These patient populations include: all pediatric patients and patients older than 65 years of age, patients who have previously had an allergic reaction to medication or IV contrast previously. Further, patients with medical a medical history including any of the following: diabetes, kidney disease, asthma, Cancer, as well as high blood pressure. Also included in this population are patients treated with chemotherapy or antibiotics, and those that have ever had dialysis.

For patients who have had a history of contrast reactions, the Radiation Oncologist may forgo the use of intravenous contrast or may prescribe pre-medication in the form of Prednisone or Benadryl. Patients may also be asked to stop taking certain medications for a fixed time prior to the CT Scan.
Check with the Radiation Oncologist before administering IV contrast. The following a rough guidelines.
- eGFR > 60 or more proceed with IV contrast
- eGFR 45 – 59 proceed with IV contrast, oral hydration recommended
- eGFR 30 - 44 proceed with IV contrast, oral and / or IV hydration required
- eGFR 15-29 consider alternative studies or withholding IV contrast
- ask the Radiation Oncologist before giving IV contrast to patients on dialysis
Potential complications from intravenous contrast include: allergic reactions in the form of itching or hives, throat swelling, difficulty breathing, as well as swelling. Temporary sensations include: feeling cold at the injections site, a surge of warmth, nausea, feeling light headed, as well as metallic taste. Care must always be exercise with patients. If in doubt, check.
- Cardiac or Respiratory Arrest
As healthcare providers; Radiation Therapists and Radiation Therapy students are required to attend BLS (Basic Life Support) training in CPR (Cardiopulmonary Recitation) to include use of an AED (Automated External Defibrillator) as well as choking intervention training.

The following review is merely an excerpt of formal training for educational as well as editorial purposes and in no way replaces the formal BLS (Basic Life Support) training requirement. http://www.heart.org/idc/groups/heart-public/@wcm/@ecc/documents/downloadable/ucm_317350.pdf
- When to Perform CPR
You find a person who appears unconscious. You must decide if CPR is needed. Tap and shake the person’s shoulder shouting are you ok. At the same time observe if the person is breathing or breathing abnormally. A person with no or abnormal breathing requires CPR.

Next, call (9-1-1) for help or direct a specific person to call for help.

- The CPR Process
CPR should be performed only on an unresponsive person. People are categorized into three groups (by age) and the process for each age group is slightly different. Adult (older than the onset of puberty)Child (1 year old till the onset of puberty)Infant (a baby under 1 year old) Remember the acronym; C-A-B. C-A-B stands for chest compressions, airway, and breathing. Begin CPR by kneeling next to the patient’s bare chest. For adults & children, place the heel of your hand on the center of the chest between the nipples. Place your other hand over the hand on the chest and interlock your fingers. Place your shoulder over the unresponsive person’s chest with your arm straight.

For infants, place two fingers on the center of the chest between the nipples.

- For adults, compress the chest 30; thirty times at a depth of at least two inches while counting aloud at the rate of at least 100 compressions a minute.
- For children, compress the chest 30; thirty times at a depth of about two inches while counting aloud at the rate of at least 100 compressions a minute.
- For infants, compress the chest 30; thirty times at a depth of about one and a half inches or a third of the chest while counting aloud at the rate of at least 100 compressions a minute.
- Press hard as well as fast allowing for full chest recoil.
- After 30 chest compressions, pinch the person’s nose, lift their chin, as well as tilt their head back. This will help open the patient’s airway.

Give two breaths each for at least a second each into the patient’s mouth for adults and children and into the mouth & nose for infants. Check to ensure the patient’s chest is rising as well as lowering or you may have to clear an airway blockage.
Continue the cycle of 30 compressions to 2 rescue breaths till the patient becomes responsive or help arrives.
- Hands-only CPR
Outside the health care setting, less than half of unresponsive people receive bystander CPR. Chest compressions alone may ensure that more unresponsive patients receive CPR from rescuers who are unable or unwilling to provide ventilations.
- 2-Rescuer CPR
2-Rescuer CPR is suitable for healthcare worker teams and others trained in 2-rescuer Basic Life Support. The chest compressions, airway, and breathing (C-A-B) CPR coordination method is similar with one team member handling compressions and the other team member handling ventilations.
Bag-mask ventilation is common in health care settings. Use the C E method. The thumb and forefinger form a C and the other three fingers under the jaw form an E.

- Choking
If a person is coughing forcefully then encourage continued coughing. A person who can’t talk, breath, and cough is choking and needs immediate help. Such a person often displays the universal choking sign.

Ask if you can help the person. If the person nods their approval, tell the person that you will use the Heimlich maneuver (abdominal thrusts). If the person is can’t talk, breath, and cough approval is assumed and you should immediately call (9-1-1) for help or direct a specific person to call for help.
Begin abdominal thrusts immediately. Stand behind the choking victim with one of your legs forward between the person’s legs. Reach around the person’s abdomen locating the victim’s navel with a finger from one hand. Make a fist with the other hand and place the thumb side of your hand against the choking person’s abdomen, above the navel. Grasp your fist with your other hand and quickly thrust inward and upward into the patient’s abdomen. You may need to thrust jerk hard enough to literally lift the choking victim off his or her feet.

Continue abdominal thrusts until the choking victim expels the obstruction or becomes unresponsive. If the choking victim becomes unresponsive, begin CPR
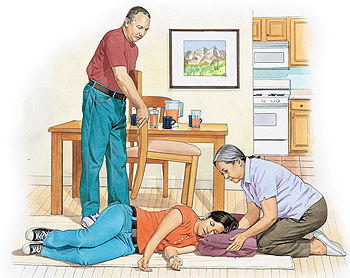
- Recovery Position
Use the recovery position for any person who is unresponsive, but breathing. The recovery position allows for drainage from the mouth and assists in maintaing an open airway.
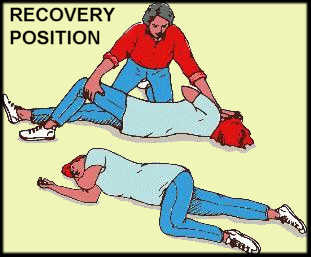
Carefully roll the person pushing on the patient’s flexed knee and lifting with your forearm while your hand stabilizes the head and neck. The patients head should be supported on their arm.
- AED (Automated External Defibrillator)
Use an AED when performing CPR if one is available. Here are some summary steps to review. After calling (9-1-1) for help or directing a specific person to call for help

- Remove clothing from the unresponsive person’s chest.
- Apply age appropriate pads to the person’s chest
- Follow the prompts on the AED
- The AED will verbally walk you through the analysis telling you “Do Not Touch The Patient”
- Shock the patient if advised (Do not touch the patient during the shock) or
- Delivery 5 cycles of CPR using C-A-B which stands for chest compressions, airway, and breathing using the ratio of 30 chest compressions to 2 breaths.
- The AED will again analyze the unresponsive person after 5 cycles of CPR
- Stop CPR if the responding patient and help them into the recovery position.
- Physical Injury or Trauma
Trauma can be defined as damage or a wound to the body caused by physical harm from an external source. The term trauma can also refer to an event that results in severe mental or emotional stress. So trauma, can be physical and / or emotional in nature.

Trauma is a medical emergency because the acute event poses an immediate risk to a person's life and health. Trauma requires an emergency medical response.
Many
external sources can cause various physical injuries. Trauma is often referred
to by the body site effected or by the external cause. Some examples of body site trauma are: head,
thorax, abdominal, as well as spinal injury. Some examples of external case
trauma are: blast injury, blunt or impact force, as well as penetrating injury.
http://www.trauma.org
Immediately after the traumatic event circulatory shock and / or emotional is typical.
Circulatory
shock means that the body is receiving an inadequate level of oxygen. Common
signs of circulatory shock may include: low blood pressure, a rapid heart beat,
cool- clammy skin, thirst, as well as poor perfusion or oxygenation of tissues.
Typical health care responses are to ask the person to lay down, elevate their
legs so more blood is available to the brain, and cover the patient with a
blanket if they are cold. http://www.nlm.nih.gov/medlineplus/ency/article/000039.htm
Common signs of emotional shock may include: denial, detachment, muteness, stress, anxiety, as well as re-experiencing the event. Re-experiencing the event in an acute response; PTSD, (Post Traumatic Stress Disorder) may take the form of dreams as well flashbacks. http://www.trauma-pages.com

Emotional
trauma may resolve itself on its own. Typical health care responses may include
counseling as well as psychotherapy. http://www.helpguide.org/mental/emotional_psychological_trauma.htm
Trauma Pictures
- Other Medical Disorders

There are many
other examples of medical disorders that may represent a medical emergency.
In
reviewing other medical disorders, we consider two examples; namely, seizures
as well as diabetic reactions here.
- Seizures
Seizures are also known as convulsions. Seizures are episodes when a person's shakes uncontrollably. During convulsion episodes, a person's muscles rapidly contract then relax repeatedly. Some seizures are different causing a person to just freeze and / or stare.
There are many possible seizure causes, but many have something to do with abnormal levels or glucose and / or sodium in the person's blood. Some examples of convulsion causes may include one or more of the following: brain lesions or anomalies, chemotherapy, drug interactions or abuse, epilepsy, fever, stroke, hypertension, as well as kidney anomalies.
Most seizures resolve themselves. Call 9-1-1 or seek help for episodes that last longer than 2 to 5 minutes. Patient's can hurt themselves during convulsions. The objective of intervention is to prevent and / or minimize injury to the person. Lay the person down. Clear the area of objects. Cushion the person's head. Loosen clothing about the neck.
Stay
with the person till back-up
healthcare help arrives. http://www.nlm.nih.gov/medlineplus/ency/article/003200.htm
- Diabetic
Reactions
Diabetic reactions are also termed insulin shock or severe hypoglycemia. Diabetes is a disease in which a person does not produce or properly use insulin. . The term hypo means low and glycemic means sugar so diabetic shock occurs due to low blood sugar levels in the cells of the body. http://www.diabetes.org
Symptoms of diabetes reactions include enhanced: frequent urination, excessive thirst, persistent hunger, weight loss, fatigue, as well as irritability.

Cells
in the body use sugar for energy. Sugar is made from carbohydrates. Insulin is
a hormone made in the pancreas that regulates how cells are able to process the
sugars in blood. When insulin is absent, cells in the body do not receive the
energy (sugars) they need to work. Diet and exercise are insulin production as
well as consumption factors.
Insulin shock is a medical emergency which can result in fainting, coma, and death. When the brain does not receive the energy (sugars) it needs, shock may occur. A diabetic reaction or hypoglycemia means that there is too much insulin in the patient's body. Insulin speeds up the lowering of blood glucose levels.
The
level of sugar can become dangerously low due to two reasons or a combination
of these two reasons. A first reason is diet. Without eating, sugars are not
being added to the blood. A second reason is exercise. Exercise means the body
uses sugars faster because of physical activity. Both diet, exercise, as well as their
combination can lead to dangerously low levels of sugar in the body. http://www.mayoclinic.org/diseases-conditions/diabetic-coma/basics/definition/con-20025691
If a patient is mildly or moderately hypoglycemic the treatment is to have them consume half a cup of fruit juice, a quarter cup of raisins, glucose tablets, hard candies (4 to 5 pieces) , or similar sugar snack items. Have the patient's blood sugar checked after 15 minutes.


In severe hypoglycemic cases, if a patient loses consciousness then a doctor may prescribe a glucagon rescue kit.

Home > Patient Care And Education > Medical Emergencies
- Ethical and Legal Aspects
- Interpersonal Communication
- Patient Assessment and Management
- Treatment Side Effects
- Blood Studies
- Dietary Counseling
- Physical Assistance and Transfer
- Patient Transfer and Movement
- Assisting Patients with Medical Equipment
- Medical Emergencies
- Infection Control
FREE Infographic What successful people believe. What successful people do
Dictionary of Cancer Terms
Need help understanding a word? Here is an electronic resource that gives meaning to Cancer terms and their usage.
StrengthsFinder 2.0
