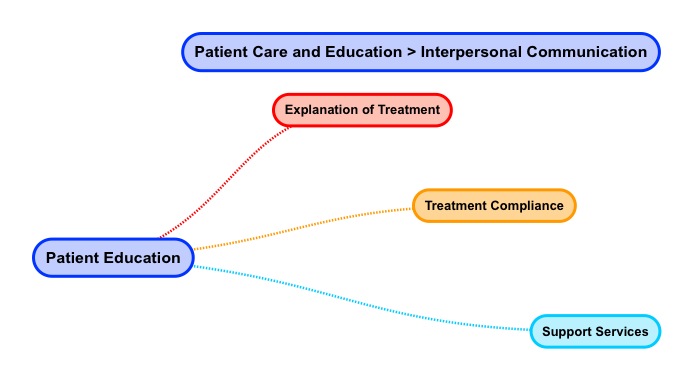
Patient Education

Home > Patient Care And Education > Interpersonal Communications > Patient Education
- Explanation of Treatment
- Treatment Compliance
- Support Services
Can we please get your advice on this one question?
Explanation of treatment, treatment compliance (positioning, skin marks), support services, (hospice, other – clergy, social services) When it comes to patient education, the way Radiation Therapists’ interact with patients is an essential part of providing quality care. Be courteous. Being courteous means being gracious or being considerate of patients.
Use the acronym AIDET (Acknowledge, Introduce, Duration, Explanation, Thank You) to guide you as you engage in patient education. Navigate to this AIDET explanation document and read it.
https://www.studergroup.com/aidet
Let’s consider a patient scenario for Mrs. Nancy Patient Jones who has been diagnosed with breast cancer and is visiting the Radiation Oncology clinic for a CT Simulation of her right breast.
A stands for Acknowledge
Acknowledge people by greeting them with a smile. Use the patient’s name in your greeting. Hello, Mrs. Nancy Patient Jones.
I stands for Introduce
Introduce yourself to patients politely. Tell them who you are as well as how you are going to help them. Escort them where they need to go instead of giving directions. My name is Betty Therapist and I will be helping you with your CT treatment planning simulation today. Let me walk you to the changing room and show you where the bathroom is.
D stands for Duration
Set expectations by telling patient how long their appointment will be. Manage and ease wait times by staying in touch with patients. Failing to inform patients about how long their visit will take may frustrate them. Informing patients about appointment duration allows them to plan for their days as well as transportation. Mrs. Jones, your simulation appointment will take around 1 hour. We are running about 20 minutes late today so we expect you will be done around 10:30 am.
E stands for Explanation
Communicate how the procedure will work. Communicate any steps a patient needs to take.
Careful planning is need before any radiation treatments can start. This planning means that you get the full benefits of radiation will minimum impacts to other parts of your body. During your CT simulation the Radiation Oncologist will map out your breast area that needs treatment. It is important that we position the angles of radiation accurately. Extra care during this session will help you get the most from your radiation therapy and ensure that your future visits run smoothly. You do not receive any treatment during this session. It’s called a “simulation” because treatment is being “simulated” and not really given.
Here is what you can expect during your CT simulation planning session.

Before Simulation
As we begin, the Radiation Oncologist will explain the advantages as well as disadvantages of radiation, planning, as well as the treatment process. The Doctor will also answer any concerns and questions you may have. The Radiation Oncologist will review the consent form and have you sign it. You will also be introduced to your treatment team.
During Simulation
In order to get the best radiation treatment, your body will be positioned during the simulation. We will use some immobilization devices like a cradle and breast board to place your head, arm, as well as hand in a fixed position. This positioning is important so we can achieve a reproducible treatment set-up each day. We will be taking photographs of the treatment set-up. We will also CT scan the area to be treated and send these detailed images of your internal organs to the treatment planning computer. Once the fields are set we will be marking you with small tattoos and using a special marking pen. The tattoos are the size of a freckle or about the size of the head of a pin. We use tattoos rather than ink marking since ink can fade as well as wash off. These tattoos guide the Radiation Therapist to align your treatment fields the same way each time your receive treatment.
After Simulation
After simulation your radiation treatment is designed or planned over next several days. This process of planning is called dosimetry. Your Radiation Oncologist works closely with the planner or Medical Dosimetrist to custom define the best arrangement and size of your treatment fields. The purpose of planning is to maximize the dose of radiation to the area that needs treatment while minimizing dose to surrounding normal tissue.
A second, planning session to verify your whole radiation plan takes place in the treatment room. X-rays are taken of each treatment field to confirm that the fields are set-up correctly. Additional markings may be made to better define the confirmed treatment fields.
With regard to Radiation Therapy support services, a variety of services are available like nutrition, hospice, as well as clergy to name a few social support services.
In terms of nutrition services, patients undergoing radiation therapy need lots of energy to heal as well as keeping their weight steady. During treatment the body requires higher amounts of nutrients just to maintain standard body functions.

Nutrition services advise patients on what foods to eat to aid in healing from the collateral cellular damage caused by radiation therapy. A patient may also be experiencing diet issues related to chemotherapy which can be addressed by nutrition services.
Another service which may be offered to radiation therapy patients is hospice. Hospice is a philosophy of care aimed at the palliation (pain relief) of seriously ill patients. Radiation therapy itself can relieve pain so hospice is a complimentary philosophy of care.

Hospice is a model of heath care that says that the right compassionate care should be provide to a patient at the right time. Care is based on a team approach to medical care, pain management, as well as emotional / spiritual support in end of life circumstances. Hospice embraces the patient right to a dignified and pain-free death where patient’s loved one receive support as well.
Another social services example is that of clergy. Clergy are people who are leaders of religion who perform religious services. Depending on the religion, these individuals may have mandates to care for the ill and to provide for end of life services.
Patient education for the radiation therapy patient may be aided by clergy. Clergy offer rituals for patients as well as their families and facilitate support in health crisis situations. Many hospitals have clergy who work with people of all faiths. Some patients may prefer their own clergy person.
Home > Patient Care And Education > Interpersonal Communications
- Ethical and Legal Aspects
- Interpersonal Communication
- Patient Assessment and Management
- Treatment Side Effects
- Blood Studies
- Dietary Counseling
- Physical Assistance and Transfer
- Patient Transfer and Movement
- Assisting Patients with Medical Equipment
- Medical Emergencies
- Infection Control
FREE Infographic What successful people believe. What successful people do
Dictionary of Cancer Terms
Need help understanding a word? Here is an electronic resource that gives meaning to Cancer terms and their usage.
StrengthsFinder 2.0