Home > Clinical Concepts in Radiation Oncology
Can we please get your advice on this one question?
- Epidermic and Etiology
- Cancer Screening
- Signs and Symptoms
- Physical Examination
- Imaging Studies
- Other Diagnostic Studies
- Brain and Spinal Cord
- Head and Neck
- Breast
- Lung
- Abdomen, Pelvis, GI and GU
- Reproductive
- Skeletal
- Miscellaneous
- Hystopathologic Types
- Histopathologic Grade
- Staging
- Chemotherapy
- Surgery
- Radiation Therapy
- Multimodality Treatment
- Tolerance Levels
- Adverse Effects
- Dose to Critical Structures
- Radiological Factors
- Biological Factors
- Medical Factors
- Other Factors
- Contribution from Other Sources
Patient Evaluation > Epidemic and Etiology
- Cancer Risk Factors
- Prevalence and Incidence
Epidemiology:
The study of the occurrence and distribution of health-related states or events in specified populations, including the study of the determinants influencing such states, and the application of this knowledge to control the health problems. Study includes surveillance, observation, hypothesis testing, analytic research, and experiments. Distribution refers to analysis by time, place, and classes or subgroups of persons affected in a population or in a society. Determinants are all the physical, biological, social, cultural, economic and behavioral factors that influence health. Health-related states and events include diseases, causes of death, behavior, reactions to preventive programs, and provision and use of health services. Specified populations are those with common identifiable characteristics. Application to control makes explicit the aim of epidemiology—to promote, protect, and restore health.
The primary “knowledge object” of epidemiology
as a scientific discipline is causes of health-related events in populations.
In the past years, the definition has broadened from concern with communicable
disease epidemics to take in all processes and phenomena related to health in
populations. Therefore epidemiology is much more than a branch of medicine
treating of epidemics.
Aetiology:
The study of all factors that may be involved in the development of a disease, including the susceptibility of the patient, the nature of the disease agent, and the way in which the patient's body is invaded by the agent.
In medicine, aetiology refers to the many factors coming together to cause an illness. It is normally the focus of epidemiological studies. A closely related term: Pathology is more specific. The aetiology of scurvy is a good example. With scurvy, the aetiology involved sailors going to see where there were no fresh vegetables. The pathology was a lack of vitamin C. The aetiology of scurvy was known way back in the time of Captain Cook. He forced his crew to eat sauerkraut every day, but he had no idea why it prevented scurvy. It was only about two centuries later - in 1926 that the pathology of scurvy was discovered.
Questions:
1. Etiology the science of,
- Study of Factors responsible for diseases
- Study of growth
- Study of statistics
- All
Answer:
- Study of factors responsible
for diseases
References:
- http://medical-dictionary.thefreedictionary.com
- http://en.wikipedia.org
- Cancer Risk Factors
- Prevalence and Incidence
Patient Evaluation > Cancer Screening
Some types of cancer can be found before they cause symptoms. Checking
for cancer (or for conditions that may lead to cancer) in people who
have no symptoms is called Screening.
Screening can help
doctors find and treat some types of cancer early. Generally, cancer
treatment is more effective when the disease is found early.
Screening tests are used widely to check for cancers of the breast, cervix, colon, and rectum:
- Breast: A mammogram is the best tool doctors have to find breast cancer early. A mammogram is a picture of the breast made with x-rays. The NCI recommends that women in their forties and older have mammograms every 1 to 2 years. Women who are at higher-than-average risk of breast cancer should talk with their health care provider about whether to have mammograms before age 40 and how often to have them.
- Cervix: The pap test (sometimes called Pap smear) is used to check cells from the cervix. The doctor scrapes a sample of cells from the cervix. A lab checks the cells for cancer or changes that may lead to cancer (including changes caused by human papillomavirus, the most important risk factor for cancer of the cervix). Women should begin having Pap tests 3 years after they begin having sexual intercourse, or when they reach age 21 (whichever comes first). Most women should have a Pap test at least once every 3 years.
- Colon and rectum: A number of screening tests are used to detect polyps (growths), cancer, or other problems in the colon and rectum. People aged 50 and older should be screened. People who have a higher-than-average risk of cancer of the colon or rectum should talk with their doctor about whether to have screening tests before age 50 and how often to have them.
- Fecal occult blood test: Sometimes cancer or polyps bleed. This test can detect tiny amounts of blood in the stool.
- Sigmoidoscopy: The doctor checks inside the rectum and lower part of the colon with a lighted tube called a sigmoidoscope. The doctor can usually remove polyps through the tube.
- Colonoscopy: The doctor examines inside the rectum and entire colon using a long, lighted tube called a colonoscope. The doctor can usually remove polyps through the tube.
- Double – contrast barium enema: This procedure involves several x-rays of the colon and rectum. The patient is given an enema with a barium solution, and air is pumped into the rectum. The barium and air improve the x-ray images of the colon and rectum.
- Digital rectal exam: A rectal exam is often part of a routine
physical exam. The health care provider inserts a lubricated, gloved
finger into the rectum to feel for abnormal areas. A digital rectal exam
allows for examination of only the lowest part of the rectum.
For the head & neck cancer some screening methods are there however it will not review persistence of sceptical origin.
Questions:
1. What is the best tool for identifying the breast cancer as early as possible?
- FNAC
- Blood test
- Mammography
- All
2. Pap test is used to screen in the cancer of,
- Oesophagus
- Colon
- Rectum
- Cervix
Answers:
- Mammography
- Cervix
References:
- www.cancer.org
- www.wikipeida.com
Patient Evaluation > Signs and Symptoms
A Sign & Symptoms are the signals of something not write in the body
and showing the illness and others abnormality in the human body.
Cancer is a group of diseases that can cause almost any sign or
symptom. The signs and symptoms will depend on where the cancer is, how
big it is, and how much it affects the organs or tissues. If a cancer
has spread (metastasized), signs or symptoms may appear in different
parts of the body.
As a cancer grows, it can begin to push on
nearby organs, blood vessels, and nerves. This pressure causes some of
the signs and symptoms of cancer. If the cancer is in a critical area,
such as certain parts of the brain, even the smallest tumor can cause
symptoms.
But sometimes cancer starts in places where it will
not cause any symptoms until it has grown quite large. One example is
cancers in the pancreas. They usually do not cause symptoms until they
grow large enough to press on nearby nerves or organs (this causes back
or belly pain). Others grow around the bile duct and block the flow of
bile. This causes the eyes and skin to look yellow (jaundice). By the
time a pancreatic cancer causes these signs or symptoms, it is usually
in an advanced stage. This means it has grown and spread beyond the
place it started -- the pancreas.
A cancer may also cause symptoms like
- Fever
- Extreme tiredness (fatigue)
- Weight loss
- Reduction in haemoglobin
This may be because cancer cells use up much of the body's energy
supply, or they may release substances that change the way the body
makes energy from food. Or the cancer may cause the immune system to
react in ways that produce these symptoms. Sometimes, cancer cells
release substances into the bloodstream that cause symptoms which are
not usually linked to cancer. For example, some cancers of the pancreas
can release substances which cause blood clots in veins of the legs.
Some lung cancers make hormone-like substances that raise blood calcium
levels. This affects nerves and muscles, making the person feel weak and
dizzy.
Questions:
1. What are the general sign and symptoms of cancer,
- Fever
- Weight loss
- Fatigue
- All
Answer:
- All
References:
- http://www.cancer.org
- http://www.nhs.uk
- www.emedicinehealth.com
Patient Evaluation > Physical Examination
Physical examination is the method to find the cancer by the victim itself before it gets severe. However, all the cancer cannot identify with the help of physical examination, only some we can identify it such as lung, breast, etc. here briefly explained about the lung and breast cancer.
Physical examination of Lung cancer:
During
the physical exam, the health professional will examine the body to help
find the cause of the symptoms. Health professional may
Take your temperature and weight to check for a fever or weight loss.
Examine your ears, eyes, nose, and throat for signs of infection.
Listen
to your heart and lungs with a stethoscope. He or she will listen for
abnormal air movement through your lungs that may indicate pneumonia or
other respiratory problems.
Examine your chest for areas of pain in your ribs or muscles.
Press or tap on your belly (abdominal palpation) to check for pain, fluid build-up, or an enlarged liver.
Examine your neck, armpits, groin, and other areas of your body to check for enlarged lymph nodes.
Physical examination of breast cancer:
In breast cases two ways are there to find the cancer one if they
doesn’t know how to examine herself means she can go for consultants or
by examining the below mentioned steps to identify it.
Step 1: Begin by looking at your breasts in the mirror with your shoulders straight and your arms on your hips. Here's what you should look for:
Step 2: Now, raise your arms and look for the same changes.
Step 3: While you're at the mirror, look for any signs of fluid coming out of one or both nipples (this could be a watery, milky, or yellow fluid or blood).

Step 4: Next, feel your breasts while lying down, using your right hand to feel your left breast and then your left hand to feel your right breast. Use a firm, smooth touch with the first few finger pads of your hand, keeping the fingers flat and together. Use a circular motion, about the size of a quarter.
Cover the entire breast from top to bottom, side to side — from your collarbone to the top of your abdomen, and from your armpit to your cleavage.
Follow a pattern to be sure that you cover the whole breast. You can begin at the nipple, moving in larger and larger circles until you reach the outer edge of the breast. You can also move your fingers up and down vertically, in rows, as if you were mowing a lawn. This up-and-down approach seems to work best for most women. Be sure to feel all the tissue from the front to the back of your breasts: for the skin and tissue just beneath, use light pressure; use medium pressure for tissue in the middle of your breasts; use firm pressure for the deep tissue in the back. When you've reached the deep tissue, you should be able to feel down to your ribcage.
Step 5: Finally, feel your breasts while you are standing or sitting. Many women find that the easiest way to feel their breasts is when their skin is wet and slippery, so they like to do this step in the shower. Cover your entire breast, using the same hand movements described in Step 4.
Questions:
1. How many months one the physical examination for the breast needs to be done?
Answer:
- 1 month
References:
- http://www.breastcancer.org
- http://www.webmd.com
Patient Evaluation > Imaging Studies
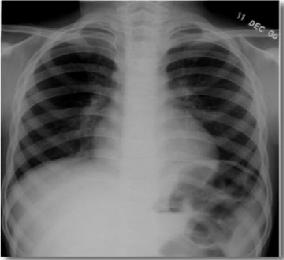
X-ray Imaging:
X-ray imaging is perhaps the most familiar
type of imaging. Images produced by X-rays are due to the different
absorption rates of different tissues. Calcium in bones absorbs X-rays
the most, so bones look white on a film recording of the X-ray image,
called a radiograph. Fat and other soft tissues absorb less, and look
gray. Air absorbs least, so lungs look black on a radiograph. The most
familiar use of X-rays is checking for broken bones, but X-rays are also
used in cancer diagnosis. For example, chest radiographs (fig:a)and
mammograms are often used for early cancer detection or to see if cancer
has spread to the lungs or other areas in the chest. Mammograms use
X-rays to look for tumors or suspicious areas in the breasts. The below figure shows the typical x-ray radiograph:
Mammography:
Conventional mammography uses X-rays to look for tumors or suspicious areas in the breasts. Digital mammography also uses X-rays, but the data is collected on computer instead of on a piece of film. This means that the image can be computer-enhanced, or areas can be magnified. Eventually, a computer could in certain appropriate situations, screen digital mammograms, theoretically detecting suspicious areas that human error might miss.
- Ct scan:
A computed tomography scan (CT scan, also called a CAT scan) uses computer-controlled X-rays to create images of the body. However a radiograph and a CT scan show different types of information. Although an experienced radiologist can get a sense for the approximate three-dimensional location of a tumor from a radiograph, in general, a plain radiograph is two-dimensional.
An arm or chest radiograph looks all the way through a body without being able to tell how deep anything is. A CT scan is three-dimensional. By imaging and looking at several three-dimensional slices of a body (like slices of bread) a doctor could not only tell if a tumor is present, but roughly how deep it is in the body. A CT scan can be three dimensional because the information about how much of the X-rays are passing through a body is collected not just on a flat piece of film, but on a computer.
The data from a CT scan can be enhanced to be more vivid than a plain radiograph. For both plain radiographs and CT scans, the patient may be given a contrast agent to drink and/or by injection to more clearly show the boundaries between organs or between organs and tumors.
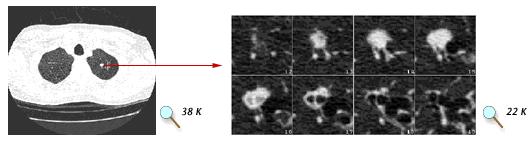
In the above figure, (Left) A 1 mm spiral CT "slice" through the mid-chest region, showing both lungs. The white spot in the right lung is a suspicious nodule that could be biopsied to see if it is cancerous. (Right) A close-up view of 8 "slices" focused on a lung nodule. Compared with a traditional X-ray, a series of CT images gives the radiologist a much better sense of nodule size and its potential threat. Images courtesy of A. P. Reeves, Cornell University.
Magnetic Resonance Imaging (MRI):
Magnetic Resonance Imaging (MRI) uses radio waves in the presence of a strong magnetic field that surrounds the opening of the MRI machine where the patient lies to get tissues to emit radio waves of their own.
Different tissues (including tumors) emit a more or less intense signal based on their chemical makeup, so a picture of the body organs can be displayed on a computer screen. Much like CT scans, MRI can produce three-dimensional images of sections of the body, but MRI is sometimes more sensitive than CT scans for distinguishing soft tissues.
Figure above shows (Top) MRI scan without contrast showing possible tumor in
the liver. (Bottom) MRI scan of the same patient using contrast. Images
courtesy of Dr. Peter Choyke, Clinical Center, NIH.
Questions:
1. Mammography is used for imaging the,
- Brain
- Chest
- Breast
- Liver
2. What is the principle behind in the x-ray image formation?
- Reflection
- Differential absorption
- Scattering
- All
Answers:
- Breast
- Differential absorption
References:
- http://imaging.cancer.gov
- http://ww5.komen.org
- http://www.elsevierscitech.com
- http://8cs25.edu.glogster.com
Patient Evaluation >Other Diagnostic Studies
Interpreting Laboratory Test Results:
A laboratory test is a medical procedure in which a sample of blood, urine, or other tissues or substances in the body is checked for certain features. Such tests are often used as part of a routine check-up to identify possible changes in a person’s health before any symptoms appear. Laboratory tests also play an important role in diagnosis when a person has symptoms. In addition, tests may be used to help plan a patient’s treatment, evaluate the response to treatment, or monitor the course of the disease over time.
Laboratory test samples are analysed to determine whether the results fall within normal ranges. They also may be checked for changes from previous tests. Normal test values are usually given as a range, rather than as a specific number, because normal values vary from person to person. What is normal for one person may not be normal for another person. Many factors (including the patient’s sex, age, race, medical history, and general health) can affect test results. Sometimes, test results are affected by specific foods, drugs the patient is taking, and how closely the patient follows pre-test instructions. That is why a patient may be asked not to eat or drink for several hours before a test. It is also common for normal ranges to vary somewhat from laboratory to laboratory.
Some laboratory tests are precise, reliable indicators of specific health problems. Others provide more general information that simply gives doctors clues to possible health problems. Information obtained from laboratory tests may help doctors decide whether other tests or procedures are needed to make a diagnosis. The information may also help the doctor develop or revise a patient’s treatment plan. All laboratory test results must be interpreted in the context of the overall health of the patient and are generally used along with other exams or tests. The doctor who is familiar with the patient’s medical history and current condition is in the best position to explain test results and their implications. Patients are encouraged to discuss questions or concerns about laboratory test results with the doctor.
Pap and HPV Testing:
- Cervical cancer screening, which includes the Pap test and HPV testing, is an essential part of a woman's routine health care because it can detect cancer or abnormalities that may lead to cancer of the cervix.
- Current guidelines recommend that women should have a Pap test every 3 years beginning at age 21. These guidelines further recommend that women ages 30 to 65 should have HPV and Pap cotesting every 5 years or a Pap test alone every 3 years. Women with certain risk factors may need to have more frequent screening or to continue screening beyond age 65.
- Women who have received the HPV vaccine still need regular cervical screening.
Prostate-Specific Antigen (PSA) Test:
- The PSA test measures the blood level of PSA, a protein that is produced by the prostate gland. The higher a man’s PSA level, the more likely it is that he has prostate cancer. However, there are additional reasons for having an elevated PSA level, and some men who have prostate cancer do not have elevated PSA.
- The PSA test has been widely used to screen men for prostate cancer. It is also used to monitor men who have been diagnosed with prostate cancer to see if their cancer has recurred (come back) after initial treatment or is responding to therapy.
- Some advisory groups now recommend against the use of the PSA test to screen for prostate cancer because the benefits, if any, are small and the harms can be substantial. None recommend its use without a detailed discussion of the pros and cons of using the test.
Biopsy:
Biopsy is also helpful to conform the disease is
whether malignant or not in all type of cancer. Sometimes all the test may show
the positive results against patients, in that biopsy all needs to be done to
avoid the confusion.
Questions:
1. Which type of cancer can be detected through the pap test?
- Lung cancer
- Brain tumour
- Abdominal cancer
- Cancer of cervix
Answer:
- Cancer of Cervix
References:
- www.cancer.gov.
Anatomy > Brain and Spinal Cord
Anatomy > Head and Neck
The head and neck region of the human body is shown in the figure figure (a) and the parts are briefly discussed below.
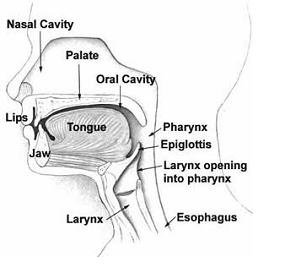
- Neck:
In our body, the neck is the part of the body including the throat region, that distinguishes the head from our torso (trunk).
- Mouth:
In our body, the mouth (oral cavity) is the entrance to the digestive system where food is broken into pieces by the teeth, saliva is excreted and local enzymes begin the digestion process.
- Nose:
In our body, the nose is an organ that protrudes on the face that houses our nostrils, which admit and expel air for respiration in conjunction with the mouth. In our body, behind the nose is the olfactory mucosa and the sinuses. Behind the nose and nasal cavity, air next passes through the pharynx, shared with the digestive system, and then into the rest of the respiratory system.
- Ear:
In our body, the Ear, is the anatomical organ that detects sound. In our body, the Ear acts as a receiver for sound, and plays a major role in both the sense of balance and body position. In our body, the ear, is part of the Auditory system, may be divided into three parts: the External ear, the Middle ear, and the Inner ear.
- Teeth:
In our body's mouth, teeth are part of the Skeletal System not counted as bones. Each tooth is made of enamel and dentin. In our body, the teeth are part of the Digestive System as an Accessory Organ along with the tongue, liver and pancreas.
- Tongue:
In our body, the Tongue is a muscular hydrostat on the floor of the mouth which manipulates food for mastication. In our body, the Tongue is the primary organ of taste, as much of the upper surface of the tongue is covered in papillae and taste buds. In our body, the Tongue is sensitive and kept moist by Saliva, and is richly supplied with nerves and blood vessels. In our body, the Tongue a secondary function of the tongue is phonetic articulation. The tongue also serves as a natural means of cleaning one's teeth.
- Face:
On our body's head, the face is a central sense organ complex, on the anterior surface of the head, including: the hair, forehead, eyebrow, eyelashes, eyes, nose, cheeks, mouth, lips, philtrum, teeth, skin, and chin.
- Facial functions:
On our body, the Face has uses of expression, appearance, and identity amongst others, including the use of different senses like olfaction, taste, hearing, and vision.
- Larynx:
In our body, the Larynx (voice box) is a hollow structure at the beginning of the trachea. The vocal cords extend across the opening of the Larynx. In our body, the Larynx (voice box) houses the vocal folds, which are an essential component of phonation. The vocal folds are situated just below where the tract of the Pharynx splits into the Trachea and the Esophagus.
- Pharynx:
In our body, the Pharynx is the part of the throat situated immediately posterior to (behind) the Mouth and naal cavity, and cranial, or superior, to the Esophagus, larynx, and trachea. In our body, the pharynx is divided into three distinct anatomic sections: the Nasopharynx, Oropharynx, and Hypopharynx.
- Functions:
In our body, the pharynx is part of the Digestive System and the Respiratory System. In our body, the pharynx is important in Vocalization.
- Salivary Gland:
Three major pairs of salivary glands supply the oral cavity: parotid, submandibular, and sublingual in the figure (b). These glands secrete saliva to assist in the process of digestion. The largest of the salivary glands are the parotid glands, which lie just below and in front of the ear. The parotid glands empty into the mouth through the parotid duct (also known as Stensen’s duct). The duct empties into the mouth through the parotid papilla, which is just opposite the maxillary second molar. The subman dibular glands are about the size of a walnut and lie on the inside of the mandible in the posterior area. They empty saliva into the mouth through the Wharton’s duct, which ends in the sublingual caruncles. The third set of glands and smallest are the sublingual glands, located on the floor of the mouth. These glands either empty directly into the mouth through the ducts of Rivinus or through the sublingual caruncles by means of the ducts of Bartholin. The ducts of the sublingual glands are similar in function to a “soaker hose.” There are also smaller minor salivary glands that are in the buccal, labial and lingual mucosa, the floor of the mouth, the posterior portion of the dorsal surface of the tongue, the soft palate, and the lateral (side) portions of the hard palate. The saliva from these glands is a mucous saliva.
Thyroid:
The thyroid gland is situated in the neck in front of
the larynx and trachea at the level of the 5th, 6h and 7th cervical and
1st thoracic vertebrae. It is a highly vascular gland that weighs about
25 g and is surrounded by a fibrous capsule. It resembles a butterfly in
shape, consisting of two lobes, one on either side of the thyroid
cartilage and upper cartilaginous rings of the trachea. The lobes are
joined by a narrow isthmus, lying in front of the trachea. The lobes are
roughly cone-shaped, about 5 cm long and 3 cm wide. Two parathyroid
glands lie against the posterior surface of each lobe and are sometimes
embedded in thyroid tissue. Figure shows the thyroid gland and
parathyroid glands fig (c)
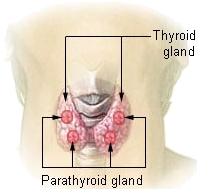
Iodine is essential for the formation of the thyroid gland hormones, thyroxine (T4) and triiodothyronine (T3). The body's main sources of iodine are seafood, vegetables grown in iodine-rich soil and iodinated table salt in the diet. The thyroid gland selectively takes up iodine from the blood, a process called iodine trapping. The parathyroid glands secrete parathyroid hormone (PTH, parathormone). Secretion is regulated by the blood level of calcium. When this falls, secretion of PTH is increased and vice versa.
Questions:
1) Larynx is called as
- Voice box
- Wind pipe
- Auditory sytem
- All
2) What is the name of hormone secreted by parathyroid?
- T3 and T4
- Bile
- Paratharmone (PTH)
- All
References:
- http://webtools.delmarlearning.com
Anatomy > Breast
Anatomy > Lung
Anatomy > Abdomen, Pelvis, GI and GU
- Esophagus, stomach, small bowel, large bowel, rectum, and anus
- Pancreas, adrenal, liver, and gallbladder Ureters, kidney, bladder, and urethra
Abdomen:
The abdomen (Fig: a) (commonly called the belly) is
the body space between the thorax (chest) and pelvis. The diaphragm
forms the upper surface of the abdomen. At the level of the pelvic
bones, the abdomen ends and the pelvis begin.
The abdomen
contains all the digestive organs, including the stomach, small and
large intestines, pancreas, liver, and gallbladder. These organs are
held together loosely by connecting tissues (mesentery) that allow them
to expand and to slide against each other. The abdomen also contains the
kidneys and spleen.
Many important blood vessels travel
through the abdomen, including the aorta, inferior vena cava, and dozens
of their smaller branches. In the front, the abdomen is protected by a
thin, tough layer of tissue called fascia. In front of the fascia are
the abdominal muscles and skin. In the rear of the abdomen are the back
muscles.
Pelvis:
The pelvis (Fig: b) is formed by the two innominate bones which articulate anteriorly at the symphysis pubis and posteriorly with the sacrum at the sacroiliac joints which are synovial joints. It is divided into two parts by the brim of the pelvis, consisting of the promontory of the sacrum and the iliopectineal lines of the innominate bones. The greater or false pelvis is above the brim and the lesser or true pelvis is below.
Differences between male and female pelvis:
The shape of the female pelvis allows for the passage of the baby
during childbirth. In comparison with the male pelvis, the female pelvis
has lighter bones, is more shallow and rounded and is generally more
roomy.
Gastro intestine & Genitourinary system (GI & GU):
Gastro intestine system: The gastrointestinal system is essentially a
long tube running right through the body, with specialized sections that
are capable of digesting material put in at the top end and extracting
any useful components from it, then expelling the waste products at the
bottom end. The whole system is under hormonal control, with the
presence of food in the mouth triggering off a cascade of hormonal
actions; when there is food in the stomach, different hormones activate
acid secretion, increased gut motility, enzyme release etc. etc.
Nutrients from the GI tract are not processed on-site; they are taken to
the liver to be broken down further, stored, or distributed.
Genitourinary
system: The kidneys are essentially regulatory organs which maintain
the volume and composition of body fluid by filtration of the blood and
selective re-absorption or secretion of filtered solutes. The kidneys
are retro-peritoneal organs (ie, located behind the peritoneum) situated
on the posterior wall of the abdomen on each side of the vertebral
column, at about the level of the twelfth rib. The left kidney is
lightly higher in the abdomen than the right, due to the presence of the
liver pushing the right kidney down.
The kidneys take their
blood supply directly from the aorta via the renal arteries; blood is
returned to the inferior vena cava via the renal veins. Urine (the
filtered product containing waste materials and water) excreted from the
kidneys passes down the fibro-muscular ureters and collects in
the bladder. The bladder muscle (the detrusor muscle) is capable of
distending to accept urine without increasing the pressure inside; this
means that large volumes can be collected (700-1000ml) without
high-pressure damage to the renal system occurring. When urine is
passed, the urethral sphincter at the base of the bladder relaxes, the
detrusor contracts, and urine is voided via the urethra.
Questions:
1. What is the capacity of urine to be collected normally?
- 600-1000ml
- 800ml
- 700-1000ml
- 2000 ml
2. At which level of the abdomen ends?
- 12 rib
- Lumbar 1
- Pelvic bone
- All
Answers:
- 700-100ml
- Pelvic bone
References:
- http://www.webmd.com
- http://www.le.ac.uk
- Ross and Wilson, Anatomy and physiology in health and illness by Anne Waugh and Allison Grant.
- Esophagus, stomach, small bowel, large bowel, rectum, and anus
- Pancreas, adrenal, liver, and gallbladder Ureters, kidney, bladder, and urethra
Anatomy > Reproductive
Anatomy > Skeletal
Skeletal system is the system of bones, associated cartilages and joints
of human body. Together these structures form the human skeleton.
Skeleton can be defined as the hard framework of human body around which
the entire body is built. Almost all the hard parts of human body are
components of human skeletal system. Joints are very important because
they make the hard and rigid skeleton allow different types of movements
at different locations. If the skeleton were without joints, no
movement would have taken place and the significance of human body; no
more than a stone.
Figure below shows the skeletal system:
Components of Human Skeleton:
Human skeleton is composed of three main components; Bones, Associated cartilages and Joints.Bones:
- Bone: Bone
is a tough and rigid form of connective tissue. It is the weight
bearing organ of human body and it is responsible for almost all
strength of human skeleton.
- Cartilages: Cartilage is also a form of connective tissue but is not as tough and rigid as bone. The main difference in the cartilage and bone is the mineralization factor. Bones are highly mineralized with calcium salts while cartilages are not.
- Joints: Joints are important components of human
skeleton because they make the human skeleton mobile. A joint occurs
between “two or more bones”, “bone and cartilage” and “cartilage and
cartilage”.
Divisions of Human Skeleton:
Human skeleton can be divided into two divisions.
- Axial Skeleton:
Axial skeleton forms the axis of human body. It consists of Skull, vertebral column and thoracic cage.
Skull: Skull is that part of human skeleton that forms the bony framework of the head. It consists of 22 different bones that are divided into two groups: bones of cranium and bones of face.
Vertebral Column: It is a flexible column of vertebrae, connecting the trunk of human body to the skull and appendages. It is composed of 33 vertebrae which are divided into 5 regions: Cervical, Thoracic, Lumbar, Sacral, and Coccygeal.
Rib Cage: It is a bony cage enclosing vital human organs formed by the sternum and ribs. There are 12 pairs of ribs that are divided into three groups: True ribs, False ribs, and Floating ribs.
- Appendicular Skeleton:
It is the skeleton of appendages of human body. It consists of Shoulder girdle, Skeleton of upper limb, Pelvic girdle and Skeleton of lower limb.
Shoulder
Girdle: It attaches the upper limb to body trunk and is formed by two
bones: clavicle and scapula.Clavicle is a modified long bone and is
subcutaneous throughout its position. It is also known as the beauty
bone. For more details on clavicle, visit:”"Scapula is a pear shaped
flat bone that contains the glenoid fossa for the formation of shoulder
joint. It possesses three important processes: Spine of scapula,
Acromion process and Coracoid process.
Skeleton of Upper
limb: The skeleton of each upper limb consists of 30 bones. These bones
are: Humerus, Ulna, Radius, Carpals (8), Metacarpals (5), Phalanges
(14).
Pelvic Girdle: There are two pelvic girdles (one for
each lower limb) but unlike the pectoral girdles, they are jointed with
each other at symphysis pubis. Each pelvic girdle is a single bone in
adults and is made up of three components: Ileum, Ischium and Pubis.
Skeleton
of Lower limb: The skeleton of each lower limb consists of 30 bones.
These bones are; Femur, Tibia, Patella, Tarsals (7), Metatarsals (5),
Phalanges (14).
Functions of human skeleton:
Human skeleton performs some important functions that are necessary for survival of human beings.
- STRENGTH, SUPPORT AND SHAPE: It gives strength, support and shape to the body. Without a hard and rigid skeletal system, human body cannot stand upright, and it will become just a bag of soft tissues without any proper shape.
- PROTECTION OF DELICATE ORGANS: In areas like the rib cage and skull, the skeleton protects inner soft but vital organs like heart and brain from external shocks. Any damage to these organs can prove fatal, therefore protective function of skeleton is very important.
- LEVERAGE FOR MOVEMENTS: Bones of the human skeleton in all parts of body provide attachment to the muscles. These muscles provide motor power for producing movements of body parts. In these movements the parts of skeleton acts like levers of different types thus producing movements according to the needs of the human body.
- PRODUCTION OF RED BLOOD CELLS: Bones like the sternum, and heads of tibia have hemopoeitic activity (blood cells production). These are the sites of production of new blood cells.
Questions:
1. Skull consists of
- 22 different bones
- 21 different bones
- 20 different bones
- 18 different bones
2. The functions of skeletal system are,
- Production of RBC’s
- Leverage of movements
- Strength, support and shape of the body
- Protect the delicate organs
- All
Answers:
- 22 different bones
- All
References:
- http://hoopmanscience.blogspot.in
- www.wikipedia.com
- http://www.mananatomy.com
Anatomy > Miscellaneous
- Lymphoma (Hodgkin’s and non- Hodgkin’s)
- Sarcomas (bone and soft tissue)
- Multiple Myeloma
- Mycosis Fungicides
- Bone marrow transplant
- Benign (heterotopic bone, keloid, AVM, etc)
Tumor Classification > Hystopathologic Types
Cancer
is not just one but many different diseases. Cancer occurs when
abnormal cells, having accumulated different mutations, divide without
control and are able to invade other tissues.
There are about 200 different types of cancer, but they all start as a
result of the out-of-control growth of abnormal cells. Cancers are
classified in two ways: by the type of tissue in which the cancer
originates (histological classification) or by the location or organ in
the body where the cancer first developed. Most people classify cancer
based on the organ in which it starts - for example, cancer that begins
in the colon is called colon cancer. However, physicians and health
professionals use histological classification because it gives a better
indication of how the cancer will behave. For instance, squamous cell
carcinoma behaves similarly whether it originates from the lung or the
prostate.
Histopathology types:
Cancer types can be grouped into histological categories, which include:
Benign Tumors:
Benign tumors are typically slow-growing and rarely spread to other
areas of the body. They often have well-defined borders, so surgical
removal can be an effective treatment. However, the location of a
benign brain tumor can have a significant impact on treatment options
and be as serious and life-threatening as a malignant tumor. Benign
brain tumors can be considered malignant if they are located in areas of
the brain that control vital functions like breathing.
- Carcinoma - cancer that originates in the skin or in tissues that line or cover internal organs. A majority (close to 90 %) of cancer are carcinoma.
- Leukemia - cancer that starts in blood-forming tissue such as bone marrow and causes large numbers of abnormal blood cells to be produced and enter the blood stream.
- Lymphoma - cancers that begin in the cells of the immune system. Lymphomas (such as Hopkins disease) are cancer of the lymphocytes (a specialized blood cell that take part in our defense against foreign material such as viruses).
- Myeloma - also a type of cancer that begins in the cells of the immune system. Myelomas are cancer of the bone marrow, particularly of the cells that produces antibodies.
- Sarcoma - cancer that begins in bone, cartilage, fat, muscle, blood vessels, or other connective or supportive tissue.
- Central nervous system specific - cancers that begin in the tissues located in the brain and central nervous system (CNS). Many types exist: glioma, blastoma, CNS lymphoma, etc.
- Mesothelioma - rare form of cancer that develops from the protective lining (called mesothelioma) that covers many of the body's internal organs such as the lining of the lungs, the heart and the abdominal cavity. It is almost always caused by exposure to asbestos.
Questions:
1. What could be the name of the cancer that occurs in soft tissue?
- Myeloma
- Mesothelioma
- Sarcoma
- Carcinoma
2. Pick out the cancer that grows in immune system?
- Lung cancer
- Lymphoma
- Glioma
- All
Answers:
- Carcinoma
- Lymphoma
References:
- www.cancer.org
- http://www.src-crs.ca
- http://www.abta.org
Tumor Classification > Histopathologic Grade
Tumor grade is a system used to classify cancer cells in terms of how
abnormal they look under a microscope and how quickly the tumour is
likely to grow and spread. Many factors are considered when determining
tumour grade, including the structure and growth pattern of the cells.
The specific factors used to determine tumour grade vary with each type
of cancer.
Histologic grade, also called differentiation,
refers to how much the tumour cells resemble normal cells of the same
tissue type. Nuclear grade refers to the size and shape of the nucleus
in tumour cells and the percentage of tumour cells that are dividing.
Tumor grade should not be confused with the stage of a cancer. Cancer
stage refers to the extent or severity of the cancer, based on factors
such as the location of the primary tumour, tumour size, number of
tumors, and lymph node involvement (spread of cancer into lymph nodes).
The tumour grade will be determined by following procedure. If a tumour
is suspected to be malignant, a doctor removes a sample of tissue or
the entire tumour in a procedure called a biopsy. A pathologist (a
doctor who identifies diseases by studying cells under a microscope)
examines the tissue to determine whether the tumour is benign or
malignant.
Below figure shows the grading system for prostate cancer
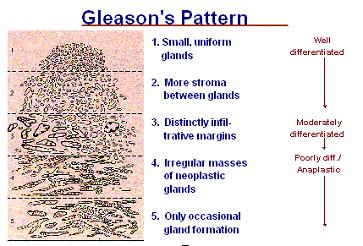
The pathologist can also determine the tumour grade and identify other characteristics of the tumour cells.
In general, a lower grade indicates (above figure) a slower-growing cancer and a higher grade indicates a faster-growing one.
- Grade I: cancer cells that resemble normal cells and aren't growing rapidly.
- Grade II: cancer cells that have features between grades I and III - they don't look like normal cells and are growing somewhat faster than normal cells.
- Grade III: cancer cells that look more abnormal and may grow or spread more aggressively
Questions:
1. Histopathologic grade helps to know about the
- Type of cancer
- Stage
- Size
- Differentiation
Answer:
- Differentiation
References:
- www.cancer.org.
- http://www.nhs.uk
- http://training.seer.cancer.gov/images/prostate/gleason_pattern.jpg
Tumor Classification > Staging
Staging
describes the severity of a person’s cancer based on the extent of the
original (primary) tumor and whether or not cancer has spread in the
body. Staging is important for several reasons:
- Staging helps the doctor plan the appropriate treatment.
- The stage can be used to estimate the person’s prognosis.
- Knowing the stage is important in identifying clinical trials that may be suitable for a particular patient.
- Staging helps health care providers and researchers exchange information about patients; it also gives them a common terminology for evaluating the results of clinical trials and comparing the results of different trials.
- Staging is based on knowledge of the way cancer progresses. Cancer cells grow and divide without control or order, and they do not die when they should. As a result, they often form a mass of tissue called a tumour. As the tumour grows, it can invade nearby tissues and organs. Cancer cells can also break away from the tumour and enter the bloodstream or the lymphatic system. By moving through the bloodstream or lymphatic system, cancer cells can spread from the primary site to lymph nodes or to other organs, where they may form new tumours. The spread of cancer is called metastasis.
- Staging systems for cancer have evolved over time. They continue to change as scientists learn more about cancer. Some staging systems cover many types of cancer; others focus on a particular type. The common elements considered in most staging systems are as follows:
- Site of the primary tumour
- Tumor size and number of tumours’
- Lymph node involvement (spread of cancer into lymph nodes)
- Cell type and tumour grade (how closely the cancer cells resemble normal tissue cells)
- The presence or absence of metastasis
The types of tests used for staging depend on the type of cancer. Tests include the following:
- Physical exams
- Imaging studies
- Laboratory tests
- Pathology reports
- Surgical reports
Questions:
1. Staging is important for to know the,
Answer:
- Extent of original tumour
References:
- www.cancer.org
- http://cancerguide.org
- www..wikipedia.com
Treatment Options >Chemotherapy
The
goal of all chemotherapy drugs is to kill the cancerous cells, while
using a dose that causes the least harm the body's healthy cells. To
achieve this goal, scientists tried to identify characteristics that are
unique to cancer cells and are not found on normal tissue. A distinct
cancer cell trait could serve as a potential target for a chemotherapy
drug and thereby spare normal tissues. One feature that is seen in most
cancer cells is that they grow at a rate faster than normal cells.
Therefore, targeting some aspect of the cell growth cycle seems
reasonable. Fast-growing cells would be affected the most and
slow-growing cells would be least disturbed. In fact, that is the basis
for many chemotherapy agents. This is apparent when considering the side
effect profiles of most chemotherapy drugs. Hair follicles, skin, and
the cells that line the gastrointestinal tract are some of the fastest
growing cells in the human body, and therefore are most sensitive to the
effects of chemotherapy. It is for this reason that patients may
experience hair loss, rashes, and diarrhea, respectively.
The human body processes and excretes all drugs through either the
liver or the kidneys. Therefore, when a patient has kidney or liver
damage, giving chemotherapy becomes precarious. Administering the
recommended amount of drug may prove to be too toxic in a patient unable
to metabolize and excrete it. The pharmacokinetics (how the body
handles a drug) for cancer patients are very complex, and chemotherapy
pharmacology is a sub specialty on its own. Unfortunately, kidney and
liver damage often result due to cancer invasion, possibly limiting the
patient's chemotherapy options.
Pharmacokinetics is further complicated in cancer patients, as they
are often taking multiple medications, some of which have overlapping
metabolic pathways and side effect profiles. An example of this
difficult situation is in the brain cancer patient. Because brain tumors
often present with seizures, many of these patients take anti-seizure
medications. Anti-seizure medications are metabolized by the liver and
affect the metabolism of many chemotherapy drugs. Dose adjustments are
an absolute necessity to avoid toxicities or sub-therapeutic dosing
(doses that are too low) in these patients.
Risks of Chemotherapy:
The side effects of chemotherapy are,
- Constipation
- Fatigue
- Hair loss
- Reduces in blood count
- Loss of apatite
- Shortness of breath
- Taste changes during cancer therapy
Long-lasting and late-developing side effects Chemotherapy drugs can also cause side effects that don't become evident until months or years after treatment. Late side effects vary depending on the chemotherapy drug, but can include:
- Damage to lung tissue
- Heart problems
- Infertility
- Kidney problems
- Nerve damage (peripheral neuropathy)
- Risk of a second cancer
Questions:
1. Choose the late effects chemotherapy from options?
- Heart problems
- Infertility
- Nerve damage
- All
Answer:
- All
References:
- www.cancer.org
- www.oncolink.org
- http://www.mayoclinic.com
Treatment Options > Surgery
Surgery
is the oldest form of cancer treatment, and for most patients, part of
the curative plan includes surgery. The most important part of the
consultation with the surgeon is a complete history and physical exam.
Before surgical resection, diagnostic and staging studies should be
performed. This helps the surgeon determine if the cancer is re sectable
(removable with surgery), and allows him or her to plan the surgical
approach. Due to improved screening techniques, many patients have
disease that is curable with surgery alone at diagnosis. In such cases,
after surgery, the patient's follow-up care includes close observation
and/or radiology and lab tests.
The goals of the surgical oncologist are to remove the cancer and an
area of healthy tissue surrounding it, also known as a clear margin or
clear excision, in order to prevent the cancer from recurring in that
area (which is called a local recurrence). Sometimes it is not possible
to remove the whole tumor, and a surgery known as "debulking" may be
done to remove as much of the tumor as possible and to relieve symptoms
such as pain, airway obstruction, or bleeding. However, the contribution
of the surgical oncologist goes beyond what is done on the day of
surgery itself. As part of the multidisciplinary care team, he or she
provides expert opinion about biopsy techniques, optimal image guidance,
the likelihood of achieving clear margins (especially in borderline
re sectable cases), and what role there is, if any, for surgical
management of more advanced disease.
For those whose cancer is not treatable, palliative surgery may be
an option to relieve pain that may be caused by the cancer. Palliative
surgery is not intended to treat or cure the cancer, or even to prolong
life, but more to lessen discomfort.
Risks of surgery:
There are risks that go with any type of medical procedure and surgery
is no exception. Success partly depends on the type of surgery you are
having and the surgeon’s experience with it. The patient’s physical
health affects the process and outcome a great deal too. What’s
important is whether the expected benefits outweigh the possible risks.
Questions:
1. If patient is diagnosed means what will be first mode of treatment?
- Chemotherapy
- Surgery
- Radiation therapy
- All
Answer:
- Surgery
References:
- http://cancer.about.com
- www.cancer.org
- http://www.oncolink.org
Treatment Options > Radiation Therapy
Radiation Therapy:
In radiation therapy (also called radiotherapy), high-energy X or gamma
rays are used to destroy the cancer cells and stop them from growing
and dividing.
Types of radiation therapy:
Treatment for cancer consists of three major parts such as surgery,
chemotherapy, and radiation therapy. In general the radiation treatment
will be prescribed alone or in combine with the surgery and
chemotherapy to achieve the extended benefit of treatment. In this type
of treatment it, affects cancer cells only in the treated area.
Radiation may deliver to the patient externally i.e. from a machine fig:
a (external radiation). It can also come from an implant (a small
container of radioactive material) placed directly into or near the
tumour (internal radiation or brachytherapy). Some patients receive
combination of both modalities for the treatment.
External Beam Radiation Therapy:
External radiation therapy is usually given on an outpatient basis in a
hospital or clinic 5 days a week for a number of weeks. Patients are
not radioactive during or after the treatment.


Above figure shows the treatment machines
Brachytherapy or Internal radiation therapy:
In brachytherapy therapy, the patient stays in the hospital for a few
days. The implant may be temporary or permanent. Because the level of
radiation is highest during the hospital stay, patients may not be able
to have visitors or may have visitors only for a short time. Once an
implant is removed, there is no radioactivity in the body. The amount of
radiation in a permanent implant goes down to a safe level before the
patient leaves the hospital.
Due to development of
technology in the field of brachytherapy now a days patients are treated
as outpatient basis like external beam therapy.
Side effects of radiation therapy:
With radiation therapy, the side effects depend on the treatment dose
and the part of the body that is treated. The most common side effects
are tiredness, skin reactions Fig: b (such as a rash or redness,
permanent pigmentation, and scarring) in the treated area, and loss of
appetite. Radiation therapy can cause inflammation of tissues and organs
in and around the body site radiated. This can cause symptoms that
depend on what organs are affected and to what degree. For example,
radiation can inflame skin to cause a burn or permanent pigmentation. It
can also irritate the colon and cause diarrhoea. Radiation therapy can
also cause a decrease in the number of white blood cells; cells that
help protect the body against infection.

Above figure shows the skin reaction due to radiation therapy
Although the side effects of radiation therapy can be unpleasant, they
can usually be treated or controlled. It also helps to know that, in
most cases, they are not permanent. To a great degree, the possible side
effects of radiation therapy depend on the location and the amount of
radiation.
Treatment Options > Multimodality Treatment
Choice of cancer treatment is influenced by several factors, including the specific characteristics of the cancer, the overall condition of the victim and whether the goal of treatment is to cure cancer, restrict the cancer from spreading, or to relieve the symptoms caused by cancer. Depending on these factors, the victim may receive one or more of the following:
- Surgery
- Chemotherapy
- Radiation therapy
- Hormonal therapy
- Targeted therapy
- Biological therapy
- Personalized Cancer Care
- Clinical Trials
- Complementary & Alternative
- Stem Cell Transplantation
All kind of therapy is having some own risks and benefits based on the fact the above treatments methods are listed.
Surgery, chemotherapy and radiation therapy are the three dominating
methods in the field of treatment for cancer. However, aforesaid methods
are also there but it is not that much successful. The most of the
cancer fall under surgery, chemotherapy and radiation therapy. In some
cases surgery is not possible at that time chemotherapy and radiation
therapy is the most preferable method of treatment.
Human body has different sensitivity among drugs used for the
treatment. Chemotherapy is successful only in specific sites such as
lung, and blood cancer etc. Because of its adverse effects during the
treatment it’s not so successful.
If the surgery and chemotherapy failed, means the last option for
treatment so far is radiotherapy. Because of emerging techniques in this
field most of the cancer detected early is cured well with 100 %
successful living rate. But it is little expensive treatment modality
than above mentioned two methods. For example head & neck, brain
tumours, abdominal, sarcomas, lymphoma’s etc. radiation are the best
treatment method till now. In some cancers after the surgery doctors’
will advise to take the radiation to prevent or to avoid recurrence and
the residual disease spreading.
Other than surgery, chemo, radiotherapy is not succeeding so much in the treatment of cancer. Because of that the popularity of the treatment methods is less to know among the people.
Questions:
1. What is the most preferable treatment method for head and neck cancers?
- Chemotherapy and target therapy
- Surgery and radiotherapy
- Surgery and stem cell transplantation
- All
Answer:
- Surgery and Radiotherapy
References:
- http://news.cancerconnect.com
Radiation Tissue Tolerance> Tolerance Levels
The proper dose of radiation depends on the type of cancer (lymphomas
are sensitive to low doses and sarcomas require high doses) and the size
of the cancer (large tumors require a higher dose.) Other factors such
as how much surgery have been performed or if chemotherapy is being
given will affect the required tumour dose.
How much is safe will
depend on which normal structures are in the way of the beam (the lens
of the eye is very sensitive but muscle tissue tolerates a very high
dose) and what percent of the organ is being hit (if most of the organ
is involved then the dose must be kept lower.) Radiation given in one
dose is more damaging than if it is divided into smaller fractions
Tolerance dose (TD) for various organs for one-third, two-thirds of
target volume and one-third of target volume at the 5% complication rate
5 years after treatment.
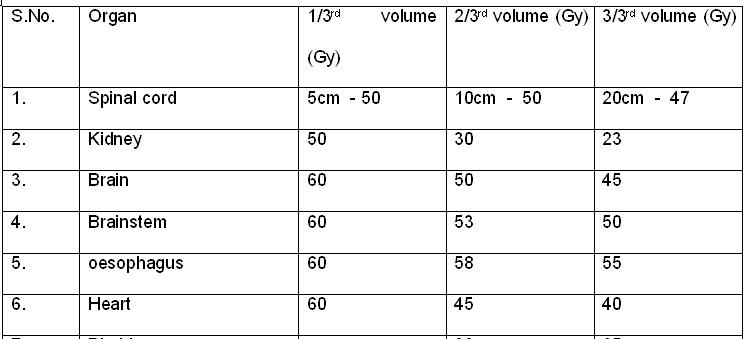
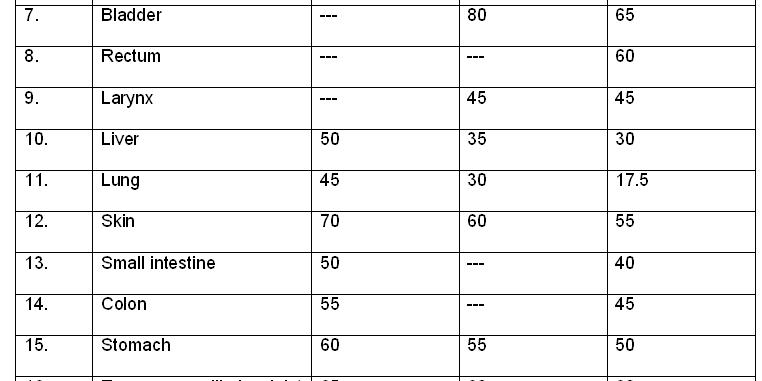
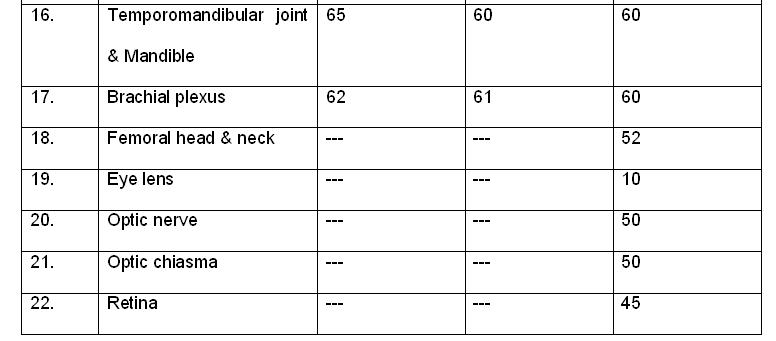
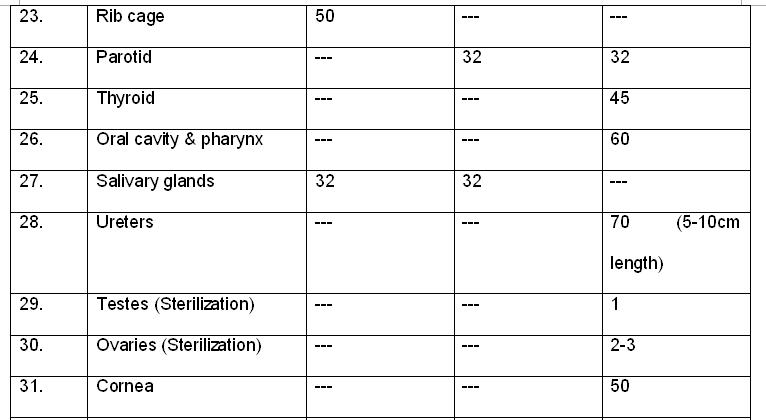
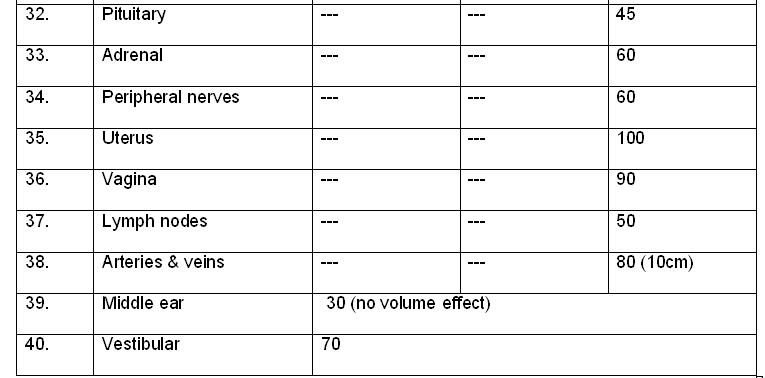
Questions:
1. What is the TD 5/5 dose if, the 3/3rd of the volume of spinal cord is irradiated?
2. What is the tolerance dose for pituitary gland?
- 50 Gy
- 75 Gy
- 45Gy
- 30 Gy
Answers:
- 47 Gy
- 45 Gy
References:
- http://www.aboutcancer.com/radiation_dose.htm
- http://www.rooj.com
- Radiobiology for the radiologist by E.J.Hall, Amato J. Giaccia
Radiation Tissue Tolerance> Adverse Effects
Radiation is used along with surgery and chemotherapy to treat cancer.
It works by damaging the DNA inside a tumour cell so that the cell is
unable to continue growing. At least half of all cancer patients will
receive radiation at some stage during their battle with cancer. Adverse
reactions may be felt as early as a few days or weeks after radiation
treatments have begun, and as long as a few years after treatments have
ended.
The three most commonly experienced side effects of radiation therapy are Fatigue:
Fatigue, or a general sense of tiredness, remains the most common
adverse side effect of radiation therapy. The fatigue probably results
due to the significant amount of energy the body utilize to heal itself
after the radiotherapy. Fatigue begins about two weeks after the therapy
begins. This side effect can last for a few weeks after treatment or up
to a year.
Skin Problems:
The skin that has been
exposed to treatment may appear red, sunburned, tan or irritated. The
skin is sensitive and should be treated as so. You can request special
creams/gels from your doctor or oncology nurse (there is one called
Radiagel, for example). Patients should avoid perfumes or scented body
lotions, tight-fitting clothing, and exposing the area to sun (during
treatment and for at least one year after). Problems with the skin will
go away after treatment ends.
Loss of Appetite:
Loss
of appetite can lead to fatigue and nutritional deficiencies. It is
important to keep up strength during any cancer treatment and food is
one of the best resources to do that. Smaller meals throughout the day
instead of three square meals help. Eating foods rich in vitamins like
fruits and veggies are essential. Appetite will increase as treatment
ends. For patients undergoing treatment for head or neck cancer (and
sometimes lung), lack of saliva can be a side effect.

Above figure, Telangiectasis in a 73-year-old woman who completed external
beam radiation therapy three and one half years earlier for an
infiltrating ductal carcinoma of the right breast (T4N2M0; stage IIIB).
Treatments included radiation to the chest wall, supraclavicular area,
and posterior axilla (5,040 cGy), followed by an electron boost to the
incision line (1,440 cGy).
Other Radiation Side Effects
This depends on what type of cancer and in which you receive treatment
on your body. Possible side effects include:Hair Loss:
Hair
loss only occurs at the site which is being treated. If you are having
radiation therapy on pelvis, there will no loss of hair on the head.
But, if they are having treatment for head and neck cancer, there will
be a experience hair loss. The good news is that in most cases, hair
does grow back after treatment.
Decreases in Blood Count:
Radiation can cause the lowering of white blood cells
and platelets. This can lead to lowered immunity to viruses and
bacteria because the white blood cells are what fights off these
attackers. Tests will be done on a regular basis to check blood
counts and treatment may be altered depending on the results. While
side effects do vary with treatment, where the radiation is being
directed will produce different side effects. For instance, treatment to
the pelvis may cause fertility problems, and treatment to the head and
neck can produce dental problems like cavities.
Questions:
1. What are the three main significant adverse effects in radiation therapy?
2. Due to radiation blood count in the body will increase or decrease
- Increase
- Decrease
- First increase and then decrease
- None
Answers:
- All
- Decrease
Reference:
- www.cancer.about.com
- http://www.livestrong.com
- http://www.aafp.org
Radiation Tissue Tolerance> Dose to Critical Structures
The dose to
critical structures plays a very important role in treatment plan
evaluation and forms a major challenging parameter in radiotherapy
treatment planning. Critical structures will vary for the site to site
in the body, for that the on the basis of site of the tumour the
critical organs doses are mentioned as follows.
Head & Neck Tumors:
The critical organs and its doses are mentioned below.
Pelvic cancers:
- Bladder : 65 Gy
- Rectum : 60 Gy
- Uterus : 90 Gy
- Vagina : 70 Gy
- Testes : Gy
- Ovaries : 2-3 Gy
- Femoral
head :52 Gy
Thorax cancers:
- Lung : 17.5 Gy
- Heart : 40 Gy
- Oesophagus : 55 Gy
- Spinal cord : 47 Gy
- Lymph nodes : 50 Gy
- Rib cage : 50 Gy
Abdominal Cancers:
- Liver : 30 Gy
- Stomach : 50 Gy
- Kidney : 23 Gy
- Small intestine : 40 Gy
- Colon : 45 Gy
- Adrenal glands : 60 Gy
- Pancreas : 30 Gy
Other sites:
- Skin : 55 Gy
- Peripheral
Nerves : 60 Gy
Questions:
1. Liver has the capability of withstand up to dose of
- 40 Gy
- 30 Gy
- 20 Gy
- All
2. What is the whole volume dose for lungs?
Answers:
- 30 Gy
- 17.5 Gy
References:
- www.cancerabout.com
- http://www.lwwoncology.com
- http://www.aapm.org
Radiation Tissue Tolerance> Radiobiological Factors
Radiobiological factors are
- Fractionation
- Dose and
- Volume
Fractionation:
The multifraction regimens commonly used in conventional radiation therapy are a consequence largely of radiobiologic experiments performed in France in the 1920s and 1930s. It was found that a ram could not be sterilized by exposing its testes to a single dose of radiation without extensive skin damage to the scrotum, whereas if the radiation was spread out over a period of weeks in a series of daily fractions, sterilization was possible without producing unacceptable skin damage.
THE FOUR Rs OF RADIOBIOLOGY
Now, more than 80 years later, we can account for the efficacy of fractionation
based on more relevant radiobiologic experiments. We can appeal to the “four
Rs” of Radiobiology,
- Repair of sublethal damage
- Reassortment of cells within the cell cycle
- Repopulation
- Reoxygenation
The basis of fractionation in radiotherapy can be understood in simple
terms. Dividing a dose into a number of fractions spares normal tissues because
of repair of sublethal damage between dose fractions and repopulation of cells
if the overall time is sufficiently long. At the same time, dividing a dose
into a number of fractions increases damage to the tumor because of reoxygenation
and reassortment of cells into radiosensitive phases of the
cycle between dose fractions.
Dose:
Radiation dose for the tumour is very to site to site and also depending on the critical structures associated with that. So many protocols has devised used widely, RTOG’s protocol are considered as most standard protocol in all over world.
Volume:
- Generally, the total dose that can be tolerated depends on the volume of irradiated tissue
- It also depend on the structural organization of the tissue in terms of the spatial arrangement of functional sub-units, FSU‟s (the nephron in the kidney, the lobule in the liver):
- If FSUs are arranged in a series, elimination of any unit is critical to the organ function (example: spinal cord)
- If FSUs are arranged in parallel, elimination of a single unit is not critical to the organ function (kidney and lung)
Questions:
1. Fractionation depends on
Answer:
- Four R’s of Radiobiology
References:
- Radiobiology for the radiologist by E.J.Hall, Amato J. Giaccia
- http://www.utoledo.edu
Radiation Tissue Tolerance> Biological Factors
Biological Factors are
- Age
- Aanatomic variation
- Medical conditions etc
Age:
Decisions about cancer treatment in the older person should be made in the same way that decisions about cancer treatment are made for younger adults and should not focus on the person’s age alone. Treatment discussions and decisions, made between the health care team and the older adult with cancer and their family, should be based on:
- The type of cancer and extent it has spread (if applicable)
- Available treatment options
- The risks and benefits of each treatment option
- The person’s assessment of his or her goals of treatment (such as curing the cancer, managing symptoms, or both) and tolerance of risk, including side effects
- The presence of medical conditions other than cancer that may put the older adult with cancer at an increased risk for treatment-related side effects or complications
- The effect of intensive treatment on the physical, emotional, and social well-being of the older adult
- The person’s concept of quality of life. Older people living with cancer often make treatment choices based on what they value most in their lives and their level of physical, emotional, and social well-being. These perceptions and decisions may differ from those of family members, friends, and caregivers.
- Emotional and social limitations, including the level of caregiver support and feelings of social connection or isolation for people with cancer who are living alone
- Financial limitations, as older adults are more likely to have limited resources and live on a fixed income, which may cause them to refuse procedures or treatment due to cost. There are ways to help relieve financial concerns.
- Spiritual beliefs, as many older adults have already come to terms with death and dying due to chronic illnesses, the loss of a spouse, or advanced age
Medical Conditions:
Medical conditions is also a prime factors suppose if a patient come with cardiac myophathy, diabetes, and high and low blood pressures etc. will cause significant problems during the treatment. If any thing goes wrong treatment would not be benefited. Because of that, complete evaluation of patient plus and its complication should be take care during treatment.
Anatomic Variation:
Anatomic variation is also a one concern in
the cases of lung , esophagus, abdomen, and gynelogical cancers. The most
suitable form of patient should be maintained by instructing the patient. Due
to the sophisticated development such as IGRT, respiratory gating this
variation can be reduced as much as earlier.
Questions:
1. Anatomic variation will reduced by using,
- Respiratory gating
- IGRT
- 4D Imaging
- All
Answer:
- All
References:
- http://www.cancer.net
Radiation Tissue Tolerance> Medical Factors
Radiation Tissue Tolerance> Other Factors
Other Factors includes
- Radio sensitizers
- Radio protectors etc
Radio protectors:
The most efficient tend to have certain structural features in common: a free SH group (or potential SH group) at one end of the molecule and a strong basic function, such as amine or guanidine, at the other end, separated by a straight chain of two or three carbon atoms. Sulfhydryl compounds are efficient radioprotectors against sparsely ionizing radiations, such as x- or γ -rays.
The mechanisms most implicated in SH-mediated cytoprotection include:
- Free-radical scavenging that protects against oxygen-based free-radical generation by ionizing radiations or chemotherapy agents such as alkylating agents.
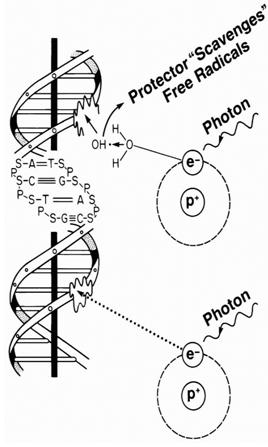
Above figure shows the schematic diagram of effect of Radioprotectors
The protective effect of sulfhydryl compounds tends to parallel the oxygen effect, being maximal for sparsely ionizing radiations (e.g., x- or γ -rays) and minimal for densely ionizing radiations (e.g., low-energy α-particles). It might be predicted that with effective scavenging of all free radicals, the largest possible value of dose-reduction factor for sparsely ionizing radiations would equal the oxygen enhancement ratio, with a value of 2.5 to 3.0.
Radiosensitizers:
Radiosensitizers are chemical or pharmacologic agents that increase the lethal effects of radiation if administered in conjunction with it. Many compounds that modify the radiation response of mammalian cells have been discovered over the years, but most offer no practical gain in radiotherapy because they do not show a differential effect between tumors and normal tissues. There is no point in employing a drug that increases the sensitivity of tumor and normal cells to the same extent.
With this all-important criterion of a differential effect, only two types of sensitizers have found practical use in clinical radiotherapy:
- Halogenated pyrimidines sensitize cells to a degree dependent on the amount of the analogue incorporated. In this case, a differential effect is based on the premise that tumor cells cycle faster and therefore incorporate more of the drug than the surrounding normal tissues.
- Hypoxic-cell sensitizers increase the radiosensitivity of cells deficient in molecular oxygen but have no effect on normally aerated cells. In this case, a differential effect is based on the premise that hypoxic cells occur only in tumors and not in normal tissues.
These two classes of sensitizers are discussed in turn. The basic strategy of all radiosensitizers . The aim is to move the tumor control curve to lower doses by sensitizing tumor cells but not affecting the normal-tissue complication curve, or at least not altering it as much. The outcome would be to increase the tumor control probability for a given level of normal-tissue complications.
Questions:
1. Choose the radioprotectors from the list,
Answer:
- Amifostine
References:
- Radiobiology for the radiologist by E.J.Hall, Amato J. Giaccia
Radiation Tissue Tolerance> Contribution from Other Sources
- Chemotherapy
- Brachytherapy
- Radiation Effect Modifiers
Home > Clinical Concepts in Radiation Oncology
FREE Infographic What successful people believe. What successful people do
Dictionary of Cancer Terms
Need help understanding a word? Here is an electronic resource that gives meaning to Cancer terms and their usage.
StrengthsFinder 2.0