Patient Evaluation
Home > Clinical Concepts In Radiation Oncology > Patient Evaluation
Nine; 9 questions out of the 55 questions in the Clinical Concepts in Radiation Oncology content area come from the Patient Evaluation sub-topic.
Can we please get your advice on this one question?
- Epidemiology and Etiology
- Cancer Screening
- Signs and Symptoms
- Physical Examination
- Imaging Studies
- Other Diagnostic Studies
- 1A Epidemiology and Etiology
As we begin our review of Clinical Concepts in Radiation Oncology, it is instructive to define the terms Epidemiology as well Etiology. The terms Epidemiology and Etiology are commonly used together. We will continue our review of patient evaluation with a consideration of Cancer Risk Factors as well as Prevalence and Incidence.
Epidemiology
Epidemiology refers to a study of
the progression and distribution of health status. Here health status includes
disease. Epidemiology is an ongoing process.
http://www.who.int/topics/epidemiology/en/ The reasoning
is that if the causes as well as the distribution of disease are understood,
then appropriate intervention actions can be taken to improve the health of
affected populations.
Etiology
Etiology is a term used to describe the causes as well as the remediation of health status. Here again, health status includes disease. http://www.nlm.nih.gov/medlineplus/ency/article/002356.htm The term etiology unlike epidemiology is also used outside the health care context to refer to the origins as well as effects of phenomena.
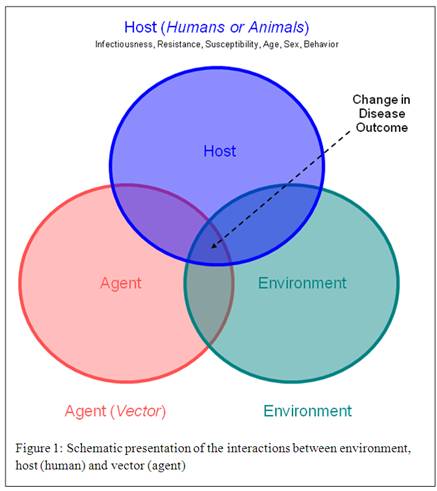
Take a look at the epidemiology / etiology diagram below which shows a relationship between: people, their environments, as well as the agents of disease.
Prevalence and Incidence
We will begin by reviewing
prevalence or the proportion of a population having a certain Cancer. We will continue by reviewing incidence;
which is, the likelihood or risk that a part of a population will develop
Cancer. Prevalence and incidence are reviewed here before Cancer risk factors
since risk factors since depend on the disease site.
An important point to reflect on
here is that the proportion of a population having a certain Cancer
(prevalence) as well as the risk that a population will develop Cancer
(incidence) depends on geographical location.
With regard to prevalence,
according to the American Cancer Society some "1,660,290 new Cancer cases are expected to be diagnosed
in 2013, and in 2013 about 580,350 Americans are projected to die of
Cancer." http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2014/index
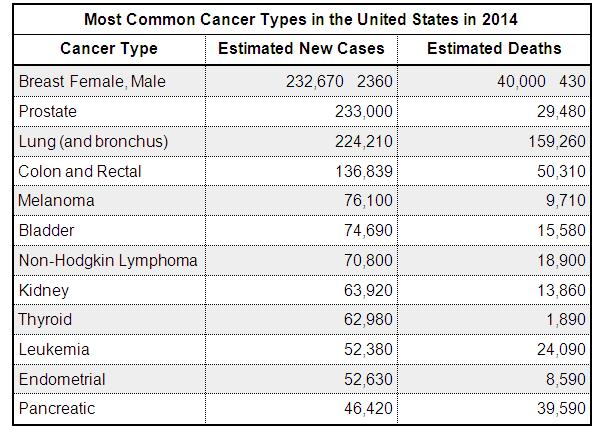
The top dozen Cancer types in the United Stare are:
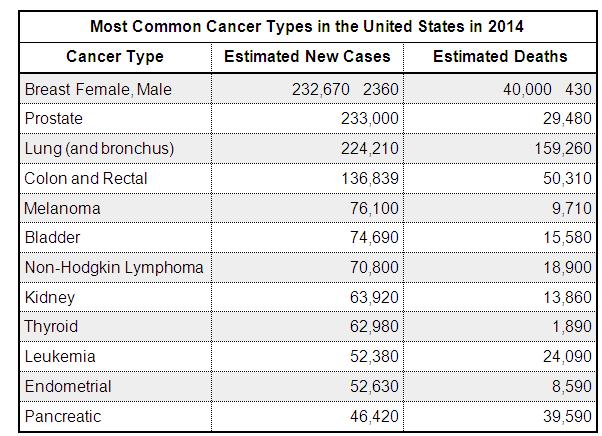
With regard to incidence, plenty of
statistics (facts & figures) are available from the American Cancer
Society by location (state), disease site, sex, race, as well as age.
Information on the probability of age interval as well as geographic
patterns are also available.
For example, here is a visual graph of the incidence of Lung Cancer deaths by geography.
Cancer Risk Factors
Cancer risk factors can be divided
into those factors which preventable and those which are not-preventable.
Cancer risk factors depend on the site of the disease. By way of review, we
will cover examples of some of the risk factors for the top dozen Cancer sites.
Breast Female http://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm
Risk factors for breast cancer and
generally divided into reproductive factors and other factors. Some
reproductive breast cancer factors are: early onset of menarche ( the first
menstrual cycle), late start of menopause, as well as never giving birth. Two of the various other risk factors include
a family history of breast cancer as well as alcohol consumption of more than a
drink each day.
Prostate http://www.cdc.gov/cancer/prostate/basic_info/risk_factors.htm
There are various risk factors for prostate cancer. Let's consider three examples; which are, age, family history, and race. As men age their risk of getting prostate cancer rises. Second, men who have a family history of prostate cancer as also at a higher risk for the disease. Third, some race / ethnicity groups (life African Americans) have a higher risk of prostate cancer incidence.
Lung http://www.cdc.gov/cancer/lung/basic_info/risk_factors.htm
There are various lung cancer risk
factors. It is no surprise that the
predominant lung cancer risk factors involve respiration plus other factors.
Smoking as well as the inhalation of other chemical like radon & asbestos
are strongly correlated to the likeliness of getting lung cancer. Indeed,
people who smoke are some 15 to 30 times more likely to get lung cancer. One
example of an "other" lung cancer risk factor is radiation. People
who have had radiation therapy to the thorax are at a higher risk of acquiring
lung cancer.
Colon and Rectal http://www.cdc.gov/cancer/colorectal/basic_info/risk_factors.htm
There are several colorectal
cancer risk factors. Colorectal risk factors can be roughly categorized as:
age, family history, and lifestyle. With
regard to age, some 90% of cases occur in people over 50 years of age. Family
history of colon and rectal disease is also a risk factor. Additionally, there are various lifestyle
factors; for examples, obesity as well as tobacco use are variables.
Melanoma http://www.cancer.gov/cancertopics/wyntk/skin/page5
Melanoma is a cancer originating
in the integumentary (skin) system. Melanoma risk factors involve various
exposures or inflammations to skin as well as family history of integumentary
disease. Lifetime sun exposure as well as tanning are examples of risk factors
related melanoma.
Bladder http://www.cancercenter.com/bladder-cancer/risk-factors/
Bladder cancer risk factors can be
categorized by gender, age, race, as well as lifestyle. With respect to gender,
men are more than three times more likely than women of being afflicted with
bladder cancer. With respect to age, most cases of bladder cancer are diagnosed
in people older than 55 years of age. With respect to race, Caucasians are at
least twice as likely to get bladder cancer than other races (African America,
Hispanic, as well as Asian). Lifestyle risk factor examples include smoking and
a low fluid intake.
Non-Hodgkin Lymphoma http://www.mcancer.org/lymphoma/risk-factors
Non-Hodgkin lymphoma is a cancer
involving organs of the immune system like lymph tissue as well as the spleen.
There are no well known causes of lymphoma. However, certain factors may
increase the risk of a person getting Non-Hodgkin lymphoma. The disease tends
to appear in people in the 60s and 70s. Non-Hodgkin Lymphoma also tends to be
more prevalent in men than in women. Further, a patient history of having the epstein-barr (EBV) virus and / or an
immune deficiency may increase the risk of a person getting Non-Hodgkin
lymphoma.
Kidney http://www.cancer.gov/cancertopics/wyntk/kidney/page4
Kidney cancer risk factors include
lifestyle as well as a family history of the disease. With regard to lifestyle,
factors like obesity, high blood pressure, as well as smoking are correlated to
a higher incidence of being afflicted with kidney cancer. Patients who have had
a family member with kidney disease are also at slightly more risk of being
afflicted.
Gender, age, exposure to radiation, as well as family history are thyroid cancer risk factors. Women are some three times more likely than men of being afflicted with thyroid cancer. Thyroid cancer also tends to manifest itself in people 25 to 75 years of age. Being exposed to head & neck radiation is also correlated to a higher incidence of thyroid cancer. Further, a family or genetic history involving the patient's medullary and / or endocrine system is a thyroid cancer risk factor.
Leukemia http://www.lls.org/diseaseinformation/leukemia/acutelymphoblasticleukemia/causesriskfactors/
Leukemia originates in the bone
marrow and is a blood cancer. There are no well known causes of Leukemia.
However, certain factors may increase the risk of a person getting Leukemia. A
family history, lifestyle, as well as environment are NOT correlated to the
incidence of Leukemia. What is known is
that, children that have had multiple x-Ray imaging studies are are a higher
risk of developing Leukemia.
Endometrial http://www.mskcc.org/cancer-care/adult/uterine-endometrial/risk-prevention-screening
Risk factors for uterine cancer
include age, lifestyle, as well as a family history. The disease tends to appear in women in the
50s and 60s. With regard to lifestyle, one example is a correlation between
obesity as well as the risk of getting uterine-endometrial cancer. Diabetes as well as hypertension are other
factors. Also, a positive family history
of uterine-endometrial cancer is a risk factor.
Pancreatic cancer risk factors can be divided into lifestyle, race, as well as family history. With respect to lifestyle risk factor examples, smoking as well as a high cholesterol diet increase chances of being afflicted with pancreatic cancer. With respect to race, some populations like African Americas as well as peoples of Jewish origin are at a higher risk of being afflicted by pancreatic cancer. Also, a positive family history of pancreatic cancer is a risk factor.
- 1B Cancer Screening
As we continue our review of Clinical Concepts in Radiation Oncology, it is instructive to review cancer screening as it applies to the top dozen Cancer types in the United States.
The top dozen Cancer types in the
United Stare are
Cancer Screening
The question we are addressing is:
What screening tests are needed to check for Cancer?
The question of who should be screened or tested for cancer is address in the following section on Clinical Concepts in Radiation Oncology > Patient Evaluation > Signs and Symptoms.
Breast Female http://www.cdc.gov/cancer/breast/basic_info/screening.htm
Breast cancer baseline screening usually takes the form of: self-breast examination, clinical breast examination, as well as mammogram.
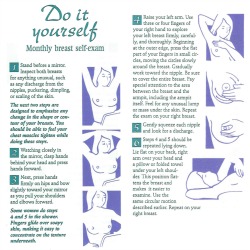
As the description suggests, self- breast examinations are done by the patient themselves while clinical breast examinations are conducted by a physician or advanced medical practitioner like a physician's assistant or nurse practitioner. Use of mammograms for screening is without a self-breast examination finding, clinical examination finding or other history is controversial.

Here is an article on the
mammogram debate. http://blogs.scientificamerican.com/cross-check/2014/02/13/consumers-must-stop-insisting-on-mammograms-and-other-ineffective-cancer-tests/
Advanced breast screening
techniques may involve breast biopsy as well as breast MRI (Magnetic Resonance
Imaging).
Prostate http://www.cdc.gov/cancer/prostate/basic_info/screening.htm
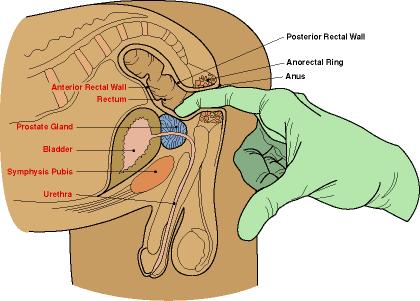
Prostate cancer baseline screening
usually takes the form of a digital rectal examination as well as PSA (Prostate Specific Antigen)
blood test. A digital rectal exam take place when a health care worker inserts
a gloved & lubricated finger into the rectum to feel for prostate size as
well as feel for lumps.
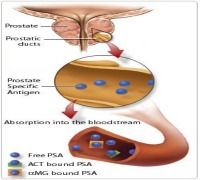
A PSA (Prostate Specific Antigen) is a protein made by the prostate measurable via a blood test. http://www.mayoclinic.org/tests-procedures/psa-test/basics/definition/prc-20013324 High PSA levels may indicate the presence of prostate cancer.
Advanced prostate screening techniques may involve Gleason biopsy as well as prostate ultrasound and prostate MRI (Magnetic Resonance Imaging).
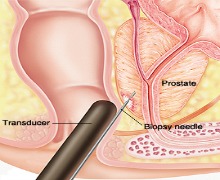
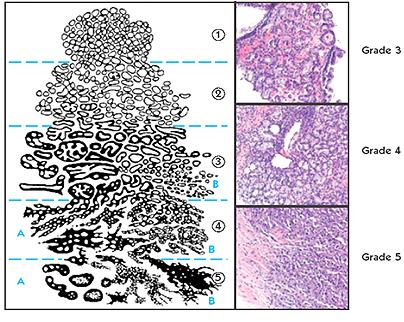
Gleason (prostate tissue) samples are obtained by trans-rectal ultrasound biopsy. Tissue samples are pathologically graded (from 1 to 5) as well as scored (from 2 to 10) based on the histology degree of cancer involvement.
Lung http://www.cancer.gov/cancertopics/pdq/screening/lung/HealthProfessional/page1
Lung cancer baseline screening is usually preceded by a finding on a diagnostic chest X-ray. Baseline lung cancer screening takes the form of a low dose CT (Computed Tomography) scan of the thorax.

Advanced lung cancer screening techniques may involve a lung biopsy.
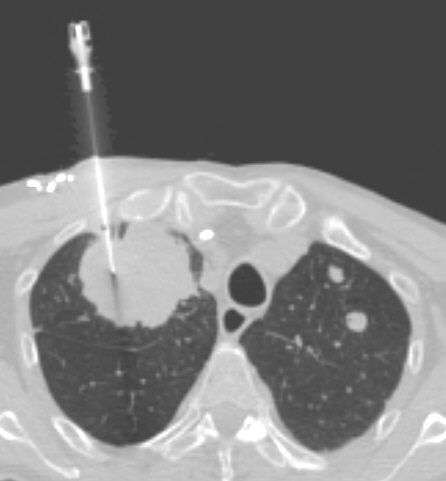
http://www.nlm.nih.gov/medlineplus/ency/article/003860.htm The lung
biopsy maybe by needle or maybe an open lung biopsy.
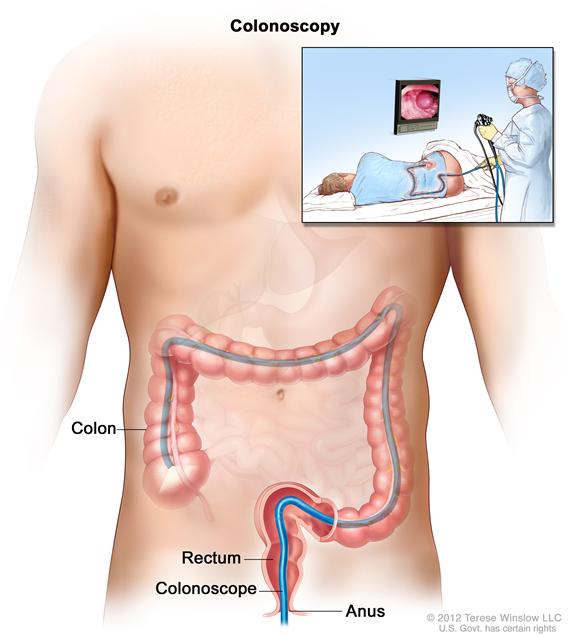
Colorectal http://www.cancer.gov/cancertopics/pdq/screening/colorectal/Patient/page3
Colorectal cancer baseline screening usually takes the form of a fecal occult blood test. (US Food and Drug :Colorectal Cancer) The purpose of the fecal (fecal meaning feces or stool) occult (occult meaning blood) test as the name suggests is meant to evaluate the presence of blood in the stool.

Advanced colorectal cancer screening may take the form of a barium enema as well as a sigmoidoscopy to visualization the inside of the rectum as well as large bowel.
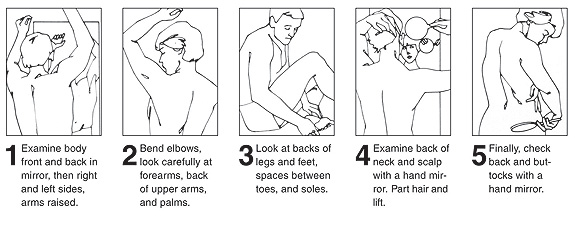
Melanoma http://www.cancerresearchuk.org/cancer-help/type/melanoma/about/melanoma-screening
Melanoma cancer baseline screening involves self-skin examination to look for the presence of abnormal skin and/ or irregular freckles or moles.
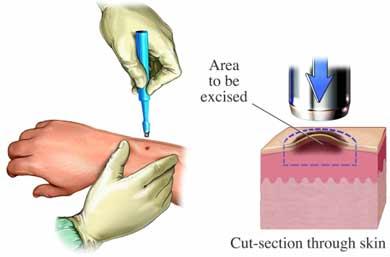
Advanced melanoma cancer examination may take the forms of a biopsy. A skin biopsy to sample the lesion may be excision (complete removal), incisional (removal of a sample), shave or punch biopsy.
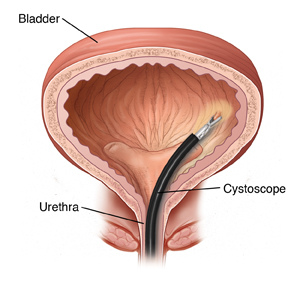
Bladder http://www.uspreventiveservicestaskforce.org/uspstf11/bladdercancer/bladcanrs.htm
Bladder cancer baseline screening
involves testing for the presence of hematuria (blood in the urine). Urinalysis
is used to test for microscopic blood in the urine.

Urine cytology is also performed
to evaluate the presence of abnormal cells in the urine. http://www.urologyhealth.org/urology/index.cfm?article=85Advanced bladder cancer screening
may involve bladder cystoscopy. http://www.nlm.nih.gov/medlineplus/ency/article/003903.htm The cystoscopy
procedure involves the insertion of a catheter thru the urethra into the
bladder to view the inside walls of the bladder.
Non-Hodgkin Lymphoma : https://www.mdanderson.org/cancer-types/non-hodgkins-lymphoma.html
There is no evidence or consensus
on baseline screening for Non-Hodgkin lymphoma at this time. The presence of
disease in the lymphatic system is hard to determine. Blood tests may show an
elevated white cell count. A physical examination may reveal swollen lymph nodes
(for examples) on the neck, underarm, and / or groin.
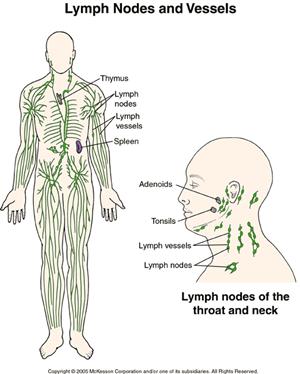
Advanced Non-Hodgkin lymphoma involve lymph node excision biopsy, PET (Positron Emission Tomography ) Scan, as well as bone marrow biopsy. http://www.nhlcyberfamily.org/diagnosis.htm Confirmation of disease from a pathologist is required.
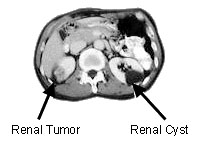
Kidney http://www.mskcc.org/cancer-care/adult/kidney/about-kidney
There is no evidence or consensus
on baseline screening for Kidney cancer at this time.
Advanced kidney cancer screening may take the form of genetic testing if there is a corroborating family history of the disease. http://www.cancer.net/cancer-types/kidney-cancer/risk-factors-and-prevention Genetic testing may indicate a higher risk of getting kidney cancer.
Screening in the form of imaging studies like X-ray, CT scan, and MRI may follow the symptomatic pursuit of causes for hematuria, swelling in the abdomen, as well as swelling in the lower extremities. A biopsy may also be performed to confirm a finding.
Thyroid : https://www.cancer.gov/types/thyroid
Baseline thyroid screening in the
form of an ultrasound may follow a finding of neck swelling. The ultrasound
examination may find a thyroid nodule. http://www.thyroid.org/what-are-thyroid-nodules/
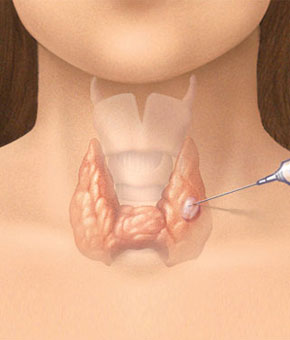
Advanced thyroid screening seeks to answer the question of if a thyroid nodule is malignant. Advanced thyroid cancer screening may take various forms. Among these tests are: CT Scan, PET Scan, CT-PET Scan, as well as fine needle aspiration. Of these tests only the fine needle aspiration yields pathologic confirmation.
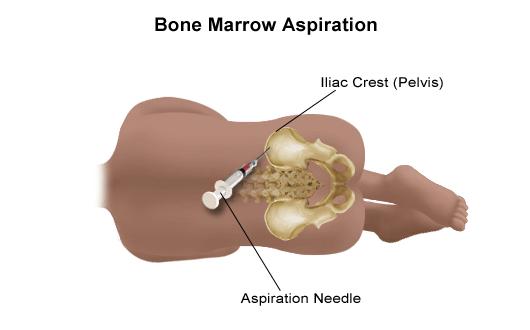
Leukemia https://www.mdanderson.org/cancer-types/leukemia.html
There is no evidence or consensus
on baseline screening for Leukemia (blood cancer) at this time. http://www.lls.org/sites/default/files/file_assets/understandingleukemia.pdf. A CBC
(Complete Blood Count) blood study may indeed indicate count as differential
anomalies.
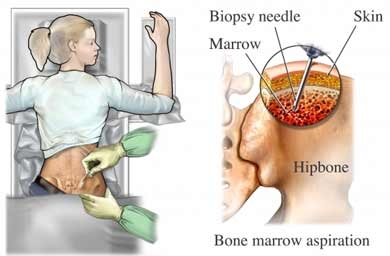
When bone marrow cells undergo leukemic changes which favor leukemia cell growth over normal cell grown blood cancers emerge. Advanced screening may take the form of a bone marrow aspiration or a bone marrow biopsy. A bone marrow aspiration and a bone marrow biopsy are similar with the aspiration sampling marrow cells while the biopsy sampling bone & marrow cells.
Endometrial http://www.cancer.gov/cancertopics/pdq/screening/endometrial/Patient/page3
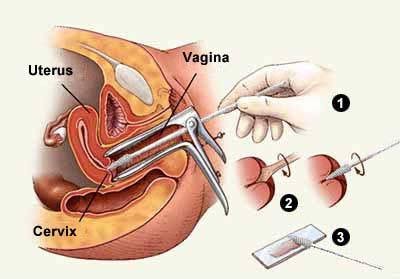
There is no consensus on baseline screening for Endometrial cancer. Endometrial cancer baseline screening actually may stem from cervix cancer screening in the form of a Pap Smear. Vaginal bleeding may be an indicator of A Pap Smear samples cells from a woman's cervix for microscopic examination.
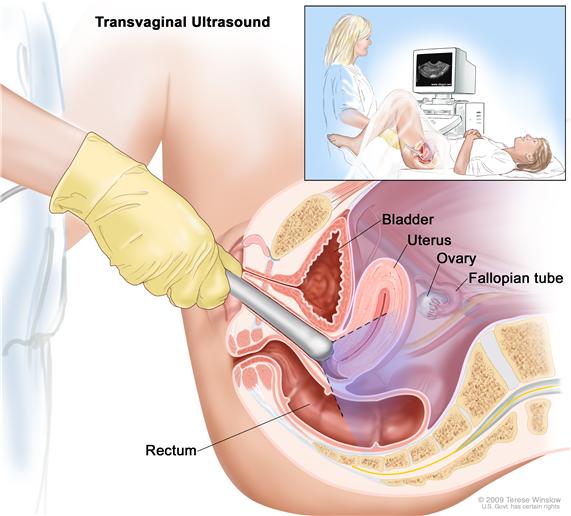
Advanced endometrial cancer screening may take
the form of translational ultrasound and endometrial sampling (biopsy). The
ultrasound examination reveals details of female anatomy including the vagina,
uterus, ovaries, as well as fallopian tubes.
Endometrial biopsy allows for microscopic tissue pathologic testing for
the presence of cancer.
Pancreas https://www.hopkinsmedicine.org/healthlibrary/conditions/adult/digestive_disorders/Pancreatic_Cancer_Diagnosis_22,PancreaticCancerDiagnosis
There is no acknowledged baseline
screening for pancreatic cancer.
Pancreatic cancer is difficult to diagnose.
Advanced pancreatic screening techniques include a variety of imaging studies, invasive examination, as well as definitive tissue sampling. With regard to imaging studies, a CT scan of the abdomen and / or MRI scan of the abdomen are able to visualize the pancreas.
Home > Clinical Concepts In Radiation Oncology > Patient Evaluation
FREE Infographic What successful people believe. What successful people do
Dictionary of Cancer Terms
Need help understanding a word? Here is an electronic resource that gives meaning to Cancer terms and their usage.
StrengthsFinder 2.0