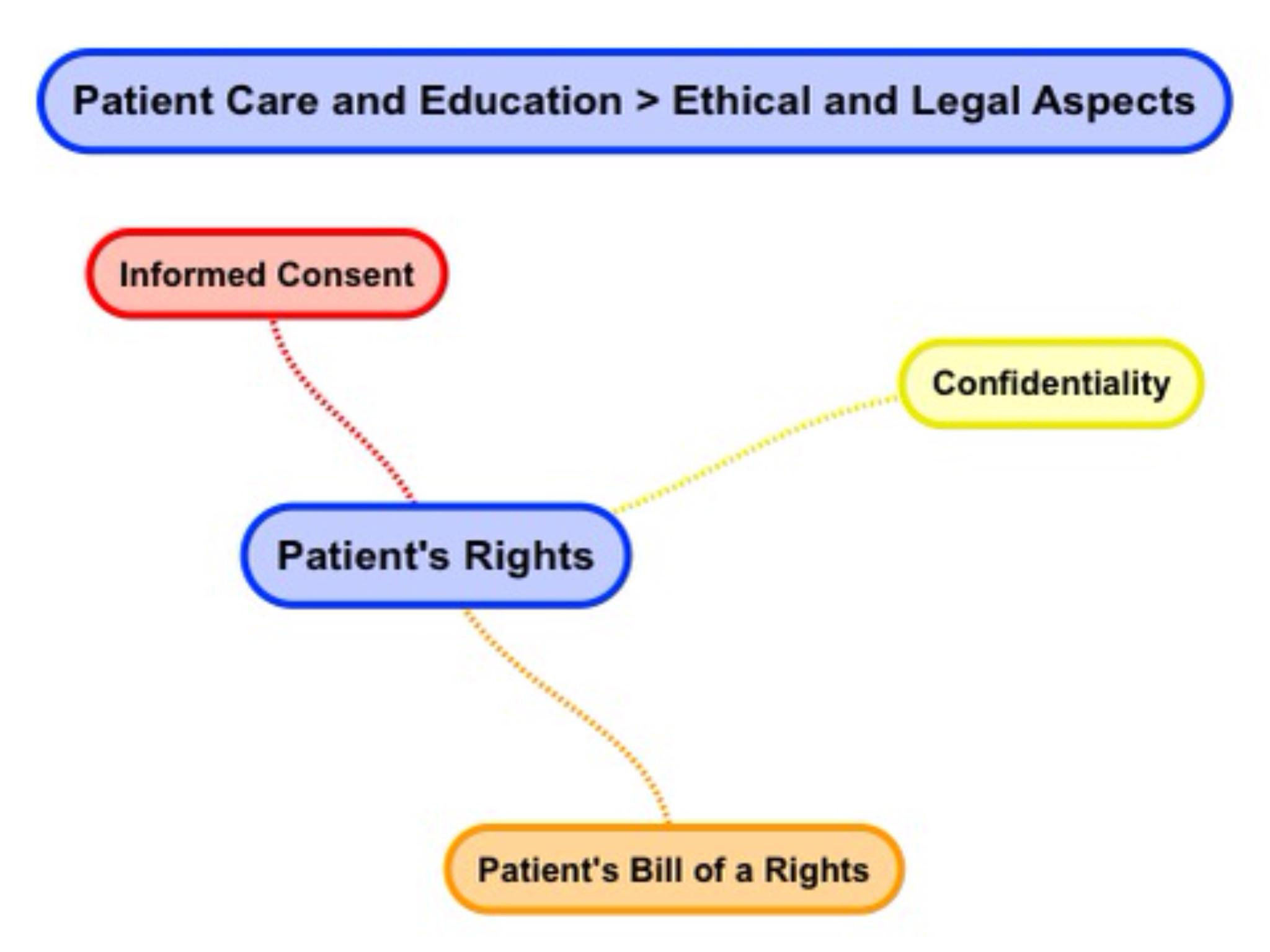
Patient's Rights

Can we please get your advice on this one question?
Home > Patient Care And Education > Patient's Rights
- Confidentiality
Let's start with the basic definition of patient’s rights. Patient’s rights refer to a list of guarantees that a person receiving medical care can expect. In our case of radiation therapy, three principal areas make up patient's rights. These principal areas are: informed consent, confidentiality, as well as additional rights. These additional rights are often referred to simply as a Patient's Bill of Rights.
The Greek Hippocratic oath is often cited as a historical basis of patient's rights. The essence of this oath is an undertaking to practice medicine honestly, to cure patients, and never to harm them.
Informed consent is the process of obtaining a patient's permission before conducting health care interventions. Patients have a right to self-determination and to agree to any medical treatment for it is given. This consent may be written, oral, as well as implied. Oral consent means that a patient verbally agrees to treatment. Implied consent means that a patient complies with the intervention.
In our case of radiation therapy, written consent is generally required for: external beam irradiation, brachytherapy, as well as radiopharmaceutical therapy. The Radiation Oncologist explains treatment options, the benefits as well as the consequences of radiotherapy treatment before obtaining written consent.
A copy of the American College of Radiology (ACR) practice guideline on informed consent - Radiation Oncology can be referenced with the link below.
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/InformedConsent-RO.pdf
Confidentiality
Next, we will define confidentiality. Confidentiality can be thought of as a set of promises or rules which limit access to patient information. The US Department of Health and Human Services is in charge of enforcing privacy rules. The Health Insurance Portability and Accountability Act of 1996 (short for HIPAA) is often equated with mandated patient confidentiality.
http://www.hhs.gov/ocr/privacy/
Simply put, health care providers must have a signed information disclosure from a patient before giving out any information on medical services provided.
Information on medical services provided to a patient is often referred to as patient health information or PHI.
The Patient Bill of Rights specifically enumerates the guarantees that a person receiving medical care can expect.
A patient has a right to health privacy. Health privacy means that you use conversational discretion when discussing patient information. For example, to not discuss patient information in public places like an elevator. Health privacy also means that medical workers are responsible for protecting the security of physical as well as electronic medical records. Only individuals directly involved in a patient's care have a right to medical records.
A patient has a right to self-determination and to agree to their extent of care. Extent of care refers to palliative care; in other words, the extent to which health care professionals will go to relieve as well as prevent the suffering of patients. A number of common legal documents specify the patient's wishes. Examples of patient determination documents are: a DNR or do not resuscitate order, as well as a five wishes statement.
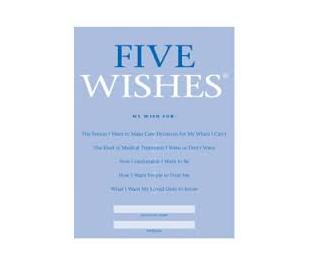
For example, a five wishes document specifies the following: Five Wishes
Wish 1: The Person I Want to Make Health Care Decisions for Me When I Can't
Wish 2: The Kind of Medical Treatment I Want or Don’t Want
Wish 3: How Comfortable I Want to Be
Wish 4: How I Want People to Treat Me
Wish 5: What I Want My Loved Ones to Know
http://www.agingwithdignity.org/catalog/product_info.php?products_id=28
A patient has a right to information about their medical condition, information in their medical record, as well as the right to designate who can access information about their medical addition. This right includes a patient's right to access information held in EHRs or Electronic Health Records.
A patient has a right to a living will as well as a healthcare proxy. A living will consists of a set of instructions that a person shares specifying what action should be taken for their health in case they are not able to take decisions because of illness. A healthcare proxy is a document the patient may use the appointed agent to make health care decisions on their behalf in cases where they may be incapacitated.
A patient also has a right to opt in or opt out of medical research participation. Information may be shared or published for research purposes if a patient has provided explicit research information consent. In such cases, patient specific information like name as well as medical record numbers are anonymized.
Understanding What Patient's Are Going Through:
Patients often experience five; 5 stages of emotions as the adjust to living with a Cancer diagnosis.
1. Denial is a common initial response. People sometimes feel that a diagnosis of Cancer is: wrong, false, or mistaken.
2. Anger shows up after a person can no longer deny their diagnosis. Common frustrations may express themselves in questions like: Why is this happening to me? and Who is to blame? and Why did this happen?
3. Bargaining means a person is trying to avoid grief by negotiating or compromising their quality of life in return for reformed lifestyle.
4. Depression may set in when a person comes to terms with their mortality. A person may avoid people. Despair may express itself in questions like: What’s the point? and Why bother? I’m going to die anyway.
5. Acceptance is a recognition of a diagnosis with reflective calmness. A person’s attitude changes to: Life goes on. and Things are going to be OK. and I am prepared. and I want to enjoy my life.
Home > Patient Care And Education > Ethical & Legal Aspects
- Ethical and Legal Aspects
- Interpersonal Communication
- Patient Assessment and Management
- Treatment Side Effects
- Blood Studies
- Dietary Counseling
- Physical Assistance and Transfer
- Patient Transfer and Movement
- Assisting Patients with Medical Equipment
- Medical Emergencies
- Infection Control
FREE Infographic What successful people believe. What successful people do
Dictionary of Cancer Terms
Need help understanding a word? Here is an electronic resource that gives meaning to Cancer terms and their usage.
StrengthsFinder 2.0